Key Takeaways
- Pyoderma is a common bacterial skin infection in dogs caused primarily by Staphylococcus pseudintermedius bacteria
- The condition is classified into three types based on infection depth: surface, superficial, and deep pyoderma
- Diagnosis requires skin cytology to confirm bacterial infection, with culture and sensitivity testing for severe or recurrent cases
- Treatment typically involves topical antimicrobial therapy for mild cases and systemic antibiotics for deep infections
- Identifying and managing underlying causes like allergies or endocrine diseases is crucial to prevent recurrence
Pyoderma is a common bacterial skin infection in dogs caused primarily by Staphylococcus pseudintermedius bacteria
The condition is classified into three types based on infection depth: surface, superficial, and deep pyoderma
Diagnosis requires skin cytology to confirm bacterial infection, with culture and sensitivity testing for severe or recurrent cases
Treatment typically involves topical antimicrobial therapy for mild cases and systemic antibiotics for deep infections
Identifying and managing underlying causes like allergies or endocrine diseases is crucial to prevent recurrence


What is Pyoderma in Dogs?
Pyoderma in dogs represents one of the most frequently encountered skin diseases in veterinary medicine. This bacterial skin infection affects dogs of all ages and breeds, literally meaning “pus in the skin.” Unlike human skin, dogs possess a thinner skin barrier and higher pH levels that increase their susceptibility to bacterial infections.
The primary causative organism behind canine pyoderma is Staphylococcus pseudintermedius, accounting for over 90% of all cases. This bacterium naturally resides on healthy canine skin but proliferates rapidly when the skin’s protective barrier becomes compromised. Understanding pyoderma’s secondary nature is crucial—it virtually always occurs due to underlying conditions that disrupt normal skin homeostasis.
What makes pyoderma particularly challenging is its tendency to recur without proper management of predisposing factors. The warm, moist environment created by skin trauma, allergic reactions, or hormonal imbalances provides ideal conditions for bacterial overgrowth syndrome to develop.
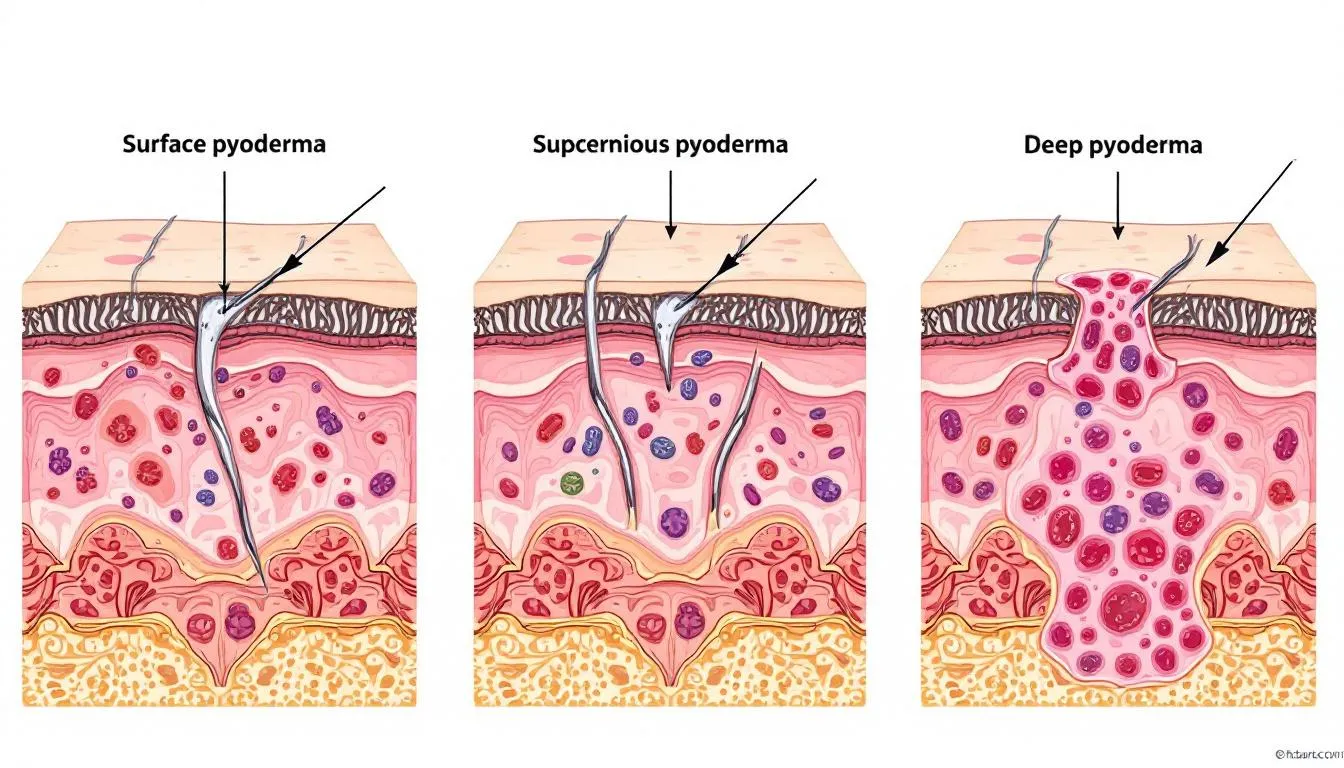
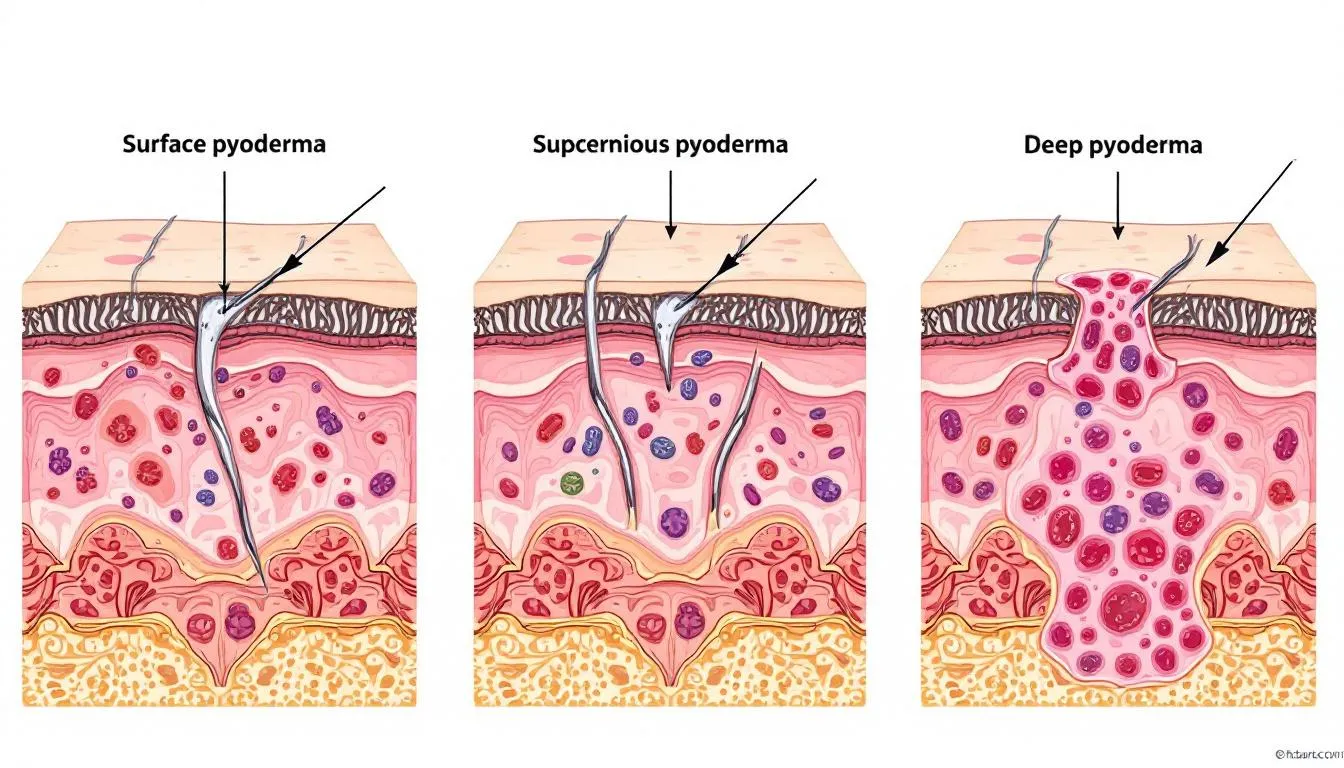
Types of Pyoderma in Dogs
Veterinary dermatologists classify pyoderma based on the depth of bacterial infection within skin layers. This classification system helps determine appropriate treatment protocols and expected recovery timelines.
Surface Pyoderma
Surface pyoderma affects only the outermost skin layer, specifically the epidermis and stratum corneum. This mildest form includes several distinct presentations that respond well to topical therapy.
Hot spots, medically termed pyotraumatic dermatitis, represent acute moist dermatitis where dogs create localized skin trauma through excessive licking or scratching. These painful, weeping lesions develop rapidly and require immediate attention to prevent deeper infection.
Skin fold pyoderma commonly affects breeds with prominent facial folds, lip folds, or body wrinkles. Bulldogs, Pugs, and Shar-Pei dogs are particularly susceptible due to their anatomical structure. The trapped moisture and reduced air circulation in these areas create perfect conditions for bacterial overgrowth.
Superficial Pyoderma
Superficial pyoderma involves the epidermis and hair follicles, creating more extensive infection than surface types. This category includes the most common presentations seen in small animal practice.
Superficial bacterial folliculitis manifests as red bumps, pus-filled lesions, and characteristic circular crusts that form when pustules rupture. Hair loss often occurs in patchy patterns, particularly noticeable in short-haired breeds where the affected skin may appear similar to hives.
Puppy pyoderma, also called impetigo, typically affects young dogs in areas with minimal hair coverage like the groin and underarms. These cases usually resolve with appropriate topical treatments and improved hygiene practices.
Deep Pyoderma
Deep pyoderma extends into the dermis and subcutaneous layers when hair follicles rupture, spreading infection deeper into tissue structures. This serious form requires aggressive treatment and may cause systemic signs of illness.
Clinical presentations include firm nodules, painful swelling, draining tracts, and characteristic purple skin discoloration. Dogs may experience lethargy, appetite loss, and behavioral changes as the infection affects their overall well-being.
Deep infections can progress to furunculosis, where multiple hair follicles become infected simultaneously, or develop into lick granulomas from chronic trauma. Callus pyoderma affects pressure points like elbows, particularly in large breed dogs that spend considerable time on hard surfaces.


Symptoms and Clinical Signs
Recognizing pyoderma’s clinical signs enables early intervention and prevents progression to more serious forms. The presentation varies significantly depending on infection depth and duration.
Common visible signs include red, raised bumps resembling pimples, circular crusts that form after pustules rupture, and flaky skin patches with varying degrees of hair loss. The intensity of itchy skin varies by pyoderma type, with superficial infections typically causing more discomfort than surface forms.
A distinctive musty odor often accompanies bacterial skin disease, particularly noticeable in skin fold areas and between toes. Chronic cases may develop progressive skin darkening and thickening due to prolonged inflammation and repeated scratching.
Breed-specific presentations require special attention. Short-haired dogs may display patchy coat patterns that appear similar to hives, while long-coated breeds might show subtle changes initially masked by their fur coverage.
Deep pyodermas present more severe symptoms including draining tracts that may produce bloody or purulent discharge, significant swelling that feels firm to touch, and systemic signs like decreased appetite or energy levels.
Causes and Risk Factors
Understanding pyoderma’s underlying causes is essential for effective treatment and prevention. As a secondary condition, bacterial infections develop when primary factors compromise the skin barrier function.
Allergic dermatitis represents the most common predisposing factor, whether from environmental allergens, food sensitivities, or flea and tick infestations. Canine atopic dermatitis creates chronic inflammation that disrupts normal skin defenses and promotes bacterial colonization.
Endocrine diseases significantly increase pyoderma risk through various mechanisms. Hypothyroidism reduces immune function and alters skin structure, while Cushing’s disease causes skin thinning and delayed healing. Thyroid disease requires specific testing and hormone replacement therapy for optimal management.
Parasitic infections, particularly demodicosis, create skin trauma that provides entry points for bacterial invasion. The immune system compromise associated with parasitic infections further promotes bacterial overgrowth.
Environmental factors play important roles in certain breeds. Skin fold anatomy in brachycephalic breeds creates warm, moist environments ideal for bacterial proliferation. Regular cleaning and drying of facial folds becomes essential preventive care for these dogs.


Diagnosis of Dog Pyoderma
Accurate diagnosis requires a systematic approach combining clinical examination, skin cytology, and selective use of bacterial culture. This three-step process ensures appropriate treatment selection and antimicrobial stewardship.
Physical examination focuses on lesion distribution, type, and severity assessment. Hair clipping may be necessary in long-coated dogs to properly visualize affected areas and evaluate the full extent of infection.
Skin Cytology
Skin cytology serves as the essential first diagnostic test for all suspected pyoderma cases, offering 93% diagnostic sensitivity for bacterial infections. This cost-effective procedure can be performed in-house with minimal equipment requirements.
Sample collection methods include impression smears from pustules or moist lesions, tape strips for dry, scaly areas, cotton swabs for hard-to-reach locations, and fine-needle aspirates for nodular lesions. Proper sampling technique significantly impacts diagnostic accuracy.
Microscopic examination identifies bacteria, particularly cocci arranged in clusters or chains, and inflammatory cells dominated by neutrophils. The presence of intracellular bacteria confirms active infection requiring antimicrobial therapy.
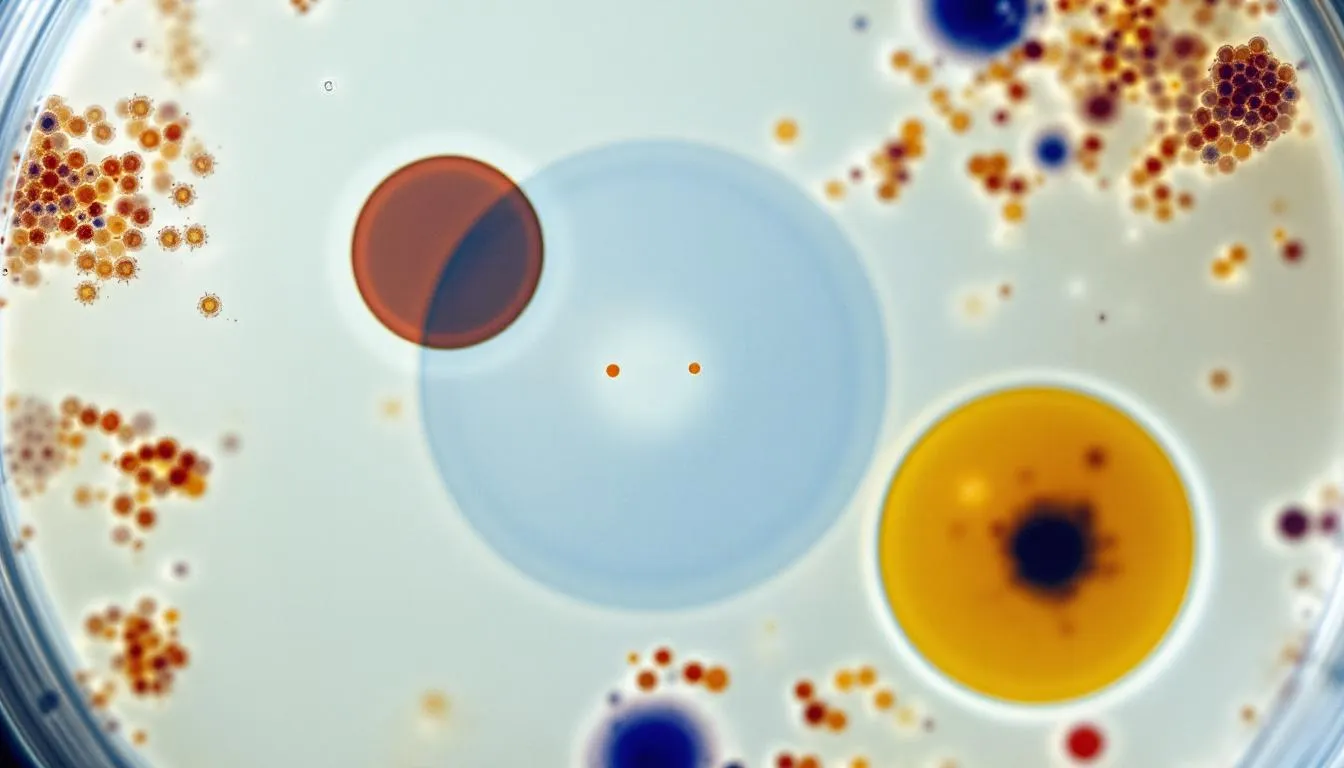
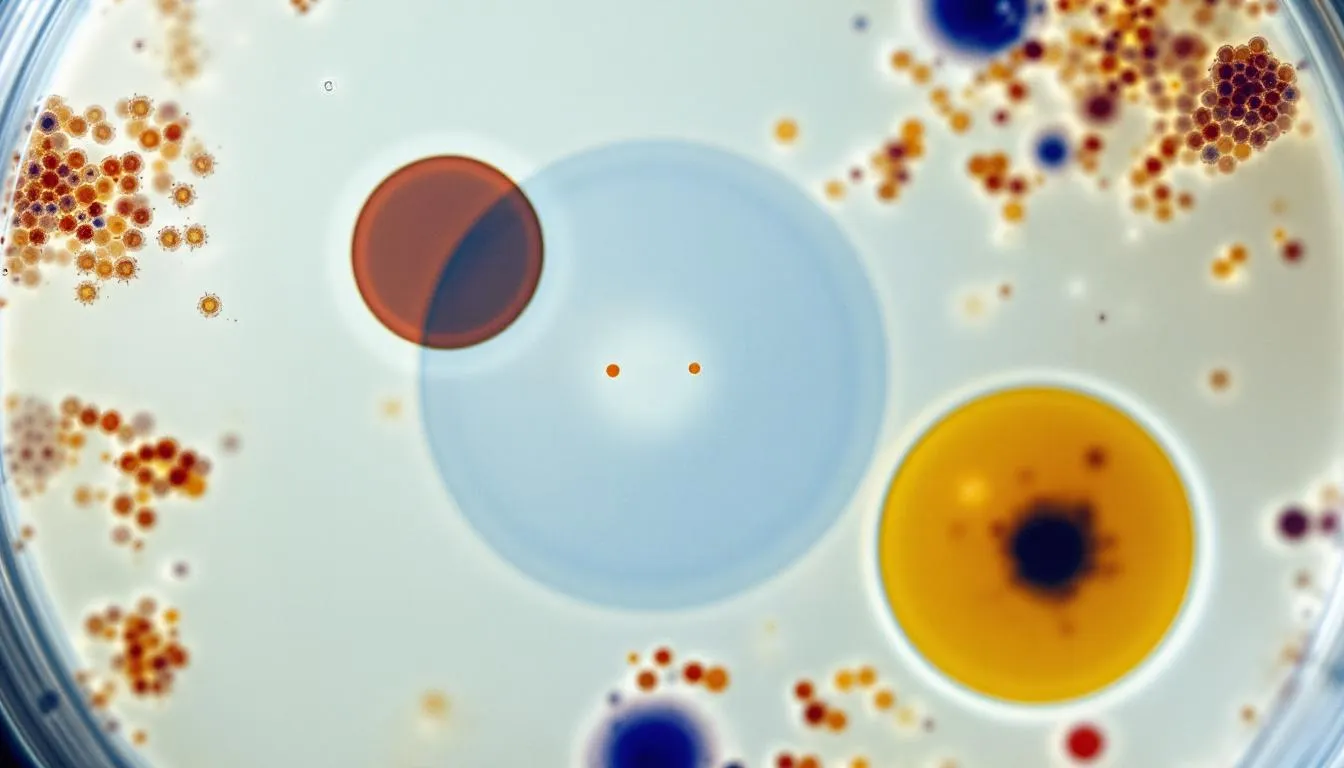
Bacterial Culture and Sensitivity Testing
Bacterial culture becomes necessary for recurrent infections, deep pyodermas, or cases showing treatment failure. This testing identifies specific bacterial species and determines antimicrobial susceptibility patterns.
Culture is particularly important when methicillin-resistant bacteria are suspected or when previous antibiotic treatment has failed. The results guide appropriate antibiotic selection and help combat antimicrobial resistance in veterinary practice.
Susceptibility testing provides crucial information for choosing effective antimicrobial agents and appropriate dosing protocols. This approach supports antimicrobial guidelines working group recommendations for responsible antibiotic use.
Additional Diagnostic Tests
Comprehensive diagnosis often requires additional testing to identify underlying causes. Skin scrapings help rule out demodicosis and other parasitic infections that may predispose to bacterial overgrowth.
Fungal cultures exclude dermatophytosis, while bacterial and fungal cultures may be performed simultaneously when multiple pathogens are suspected. These tests prevent misdiagnosis and ensure targeted treatment approaches.
Allergy testing becomes valuable when pyoderma appears linked to allergic dermatitis. Blood tests for endocrine diseases like hypothyroidism or Cushing’s disease help identify systemic conditions requiring concurrent treatment.
Treatment Options for Dog Pyoderma
Effective treatment strategies depend on pyoderma type, infection severity, and identification of underlying causes. Successful outcomes require addressing both the bacterial infection and predisposing factors simultaneously.
Elizabethan collars provide essential support during treatment by preventing licking and allowing proper healing. This simple intervention significantly improves treatment success rates across all pyoderma types.
Topical Antimicrobial Therapy
Topical therapy serves as first-line treatment for surface and superficial pyoderma cases. These treatments offer several advantages including reduced systemic antibiotic exposure, effectiveness against resistant bacteria, and excellent safety profiles.
Medicated shampoos containing chlorhexidine, benzoyl peroxide, or ethyl lactate provide broad-spectrum antimicrobial activity. Proper application requires adequate contact time, typically 10-15 minutes, and thorough rinsing to prevent skin irritation.
Non-rinse topical treatments including mousses, wipes, and sprays offer convenient options for localized skin infections. These products provide residual antimicrobial activity lasting up to 10 days with some formulations.
Antibacterial shampoos require specific application techniques for optimal effectiveness. Hair clipping improves product contact with affected skin, while proper dilution prevents irritation in sensitive dogs.
Systemic Antibiotic Treatment
Oral antibiotics become necessary for deep infections or refractory superficial cases that fail to respond to topical treatments alone. Systemic antimicrobial therapy provides better tissue penetration for deeper infections.
First-choice antibiotics effective against Staphylococcus spp include amoxicillin-clavulanate, cephalexin, and clindamycin. These medications show excellent activity against most canine skin pathogens and have established safety records.
Second-choice antimicrobial agents are reserved for culture-confirmed resistant infections or when first-line drugs prove inappropriate. These include fluoroquinolones and other broad-spectrum antibiotics requiring careful stewardship.
Treatment duration must extend 7-14 days beyond clinical cure to prevent antibiotic resistance development. This approach, recommended by antimicrobial guidelines working group protocols, ensures complete bacterial elimination.
Treatment Duration by Pyoderma Type
Surface pyoderma typically responds to 1-2 weeks of topical therapy when underlying causes are addressed. Short treatment courses reduce the risk of developing resistant bacteria while maintaining effectiveness.
Superficial pyodermas usually require 3-4 weeks of systemic antibiotics to achieve clinical cure. Premature discontinuation frequently leads to treatment failure and potential resistance development.
Deep infections may require months of antibiotic therapy with regular monitoring for treatment response and adverse effects. These cases benefit from bacterial culture guidance and close veterinary supervision.
Antibiotic Resistance Concerns
The increasing prevalence of methicillin-resistant Staphylococcus pseudintermedius (MRSP) presents significant challenges in companion animal infectious diseases management. Understanding resistance patterns helps guide appropriate treatment decisions.
Risk factors for resistant bacteria include repeated antibiotic use, chronic skin disease, and previous hospitalization. Dogs with recurrent pyoderma face higher risks of developing multidrug-resistant infections requiring specialized treatment approaches.
Reserved antibiotics should only be used for confirmed multidrug-resistant infections based on culture results. This approach preserves these important drugs for cases where they are truly necessary.
Topical treatments remain effective against many resistant bacteria and offer valuable alternatives to systemic therapy. These products bypass many resistance mechanisms and provide excellent local antimicrobial activity.
The importance of antimicrobial stewardship in veterinary medicine cannot be overstated. Responsible antibiotic use protects both individual patients and the broader population from resistance development.
Managing Underlying Causes
Successful long-term management requires identifying and treating the underlying cause of skin barrier compromise. Without addressing these predisposing factors, pyoderma will likely recur despite appropriate antimicrobial therapy.
Allergy management involves multiple approaches including anti-inflammatory medications, antihistamines, and immunotherapy for environmental allergens. Food allergies may require elimination diets and novel protein sources to identify trigger ingredients.
Endocrine disease treatment typically involves hormone replacement therapy for hypothyroidism or specific medications for Cushing’s disease. These systemic conditions require ongoing monitoring and dose adjustments to maintain optimal control.
Parasite control through regular preventive treatments helps eliminate fleas, ticks, and mites that can trigger allergic reactions or directly damage skin integrity. Year-round prevention is often necessary in many geographic regions.
Environmental modifications prove particularly important for breeds prone to skin fold infections. Daily cleaning and thorough drying of facial folds, lip folds, and body wrinkles prevents moisture accumulation and bacterial proliferation.
Preventing Pyoderma Recurrence
Prevention strategies focus on maintaining skin health and controlling predisposing factors. Regular use of antimicrobial shampoos as maintenance therapy can help prevent recurrent infections in susceptible dogs.
Proper skin fold care requires daily attention in predisposed breeds. Gentle cleaning with appropriate products followed by thorough drying helps maintain healthy skin conditions in these areas.
Weight management in overweight dogs reduces skin fold problems and improves overall health. Excess weight creates additional skin folds and increases friction in problem areas.
Environmental allergen control and dietary management for allergic dogs helps reduce the inflammatory conditions that predispose to bacterial infections. Air filtration, regular cleaning, and allergen avoidance strategies prove beneficial.
Regular veterinary monitoring every 6-12 months allows early detection of recurring problems and adjustment of prevention protocols. This proactive approach prevents minor issues from developing into serious infections.
Prognosis and Recovery
The prognosis for most pyoderma cases is excellent when appropriate treatment addresses both the infection and underlying causes. Uncomplicated surface and superficial infections typically resolve completely with proper therapy.
Good outcomes depend on client compliance with treatment protocols and follow-up recommendations. Premature treatment discontinuation remains the most common cause of treatment failure and recurrence.
Deep infections require longer treatment periods but generally respond well to appropriate antibiotic therapy and supportive care. Some cases may develop permanent scarring or skin changes, but functional recovery is usually complete.
Recurrent cases need ongoing management strategies that may include maintenance topical therapy, environmental modifications, and treatment of chronic underlying conditions like allergies or endocrine diseases.
Regular veterinary follow-up appointments allow monitoring of treatment response and early detection of any complications. This ongoing partnership ensures optimal outcomes for affected dogs.
Is Pyoderma Contagious?
The risk of transmission between dogs in the same household remains relatively low for most pyoderma cases. However, some bacterial strains, particularly Staphylococcus aureus, may pose transmission risks under certain circumstances.
Rare but possible transmission to humans can occur, especially with certain bacterial strains. Immunocompromised individuals and children face higher risks and should take appropriate precautions around infected animals.
Good hygiene practices including thorough handwashing after handling affected dogs and proper wound care help prevent potential transmission. These simple measures significantly reduce any risk to human family members.
Regular cleaning of pet bedding, toys, and living areas helps eliminate environmental bacterial contamination. Using appropriate disinfectants and maintaining clean environments supports treatment success.
Dogs with deep pyodermas or draining lesions may harbor bacteria that pose greater transmission risks. These cases require more stringent hygiene measures and careful handling during treatment.
When to See a Veterinarian
Any suspected bacterial skin infection requires professional veterinary diagnosis to ensure appropriate treatment selection. Early intervention prevents progression to more serious forms and improves treatment outcomes.
Worsening symptoms despite initial treatment attempts indicate the need for veterinary evaluation and possible treatment modification. This may include bacterial culture, medication changes, or investigation for underlying causes.
Recurrent skin infections occurring more than once yearly suggest underlying conditions requiring professional investigation. These cases benefit from comprehensive diagnostic workups to identify predisposing factors.
Signs of deep infection including draining tracts, severe swelling, or systemic illness require immediate veterinary attention. These serious cases may need hospitalization and intensive treatment protocols.
Culture and sensitivity testing becomes necessary for appropriate antibiotic selection in complicated cases. This testing ensures effective treatment while supporting responsible antimicrobial use.
FAQ
How long does it take for pyoderma to heal in dogs?
Surface pyoderma typically heals within 1-2 weeks with topical treatment, superficial pyoderma requires 3-4 weeks of antibiotics, while deep pyoderma may need months of therapy depending on severity and underlying causes. Treatment should always continue 7-14 days beyond visible improvement to ensure complete bacterial elimination and prevent recurrence.
Can I use human antibiotics to treat my dog’s pyoderma?
No, never use human antibiotics for dogs as they can be toxic and inappropriate dosing may worsen antibiotic resistance. Dogs require veterinary-specific medications with proper dosing based on their weight and condition. Always consult a veterinarian for proper diagnosis and prescription of veterinary-approved medications that are safe and effective for canine use.
Why does my dog keep getting pyoderma despite treatment?
Recurrent pyoderma indicates an underlying cause that hasn’t been identified or properly managed, such as allergies, endocrine diseases, or immune disorders. Your veterinarian needs to investigate and treat these primary conditions through allergy testing, blood work for hormonal imbalances, or immune system evaluation to break the cycle of recurring infections.
Are certain dog breeds more prone to pyoderma?
Yes, breeds with skin folds like Bulldogs, Pugs, Shar-Pei, and Spaniels are predisposed to skin fold pyoderma due to trapped moisture and reduced air circulation. Breeds prone to allergies or endocrine diseases may develop other forms of pyoderma more frequently. Additionally, dogs with compromised immune systems or those taking certain medications face increased risk.
Can I prevent pyoderma in my dog?
While not always preventable, you can reduce risk by maintaining good hygiene, managing allergies through proper diet and environmental control, controlling parasites with regular preventive treatments, keeping skin folds clean and dry, and addressing underlying health conditions promptly with veterinary care. Regular grooming and maintaining a healthy weight also help prevent skin problems that can lead to bacterial infections.
FAQ
How long does it take for pyoderma to heal in dogs?
Surface pyoderma typically heals within 1-2 weeks with topical treatment, superficial pyoderma requires 3-4 weeks of antibiotics, while deep pyoderma may need months of therapy depending on severity and underlying causes. Treatment should always continue 7-14 days beyond visible improvement to ensure complete bacterial elimination and prevent recurrence.
Can I use human antibiotics to treat my dog’s pyoderma?
No, never use human antibiotics for dogs as they can be toxic and inappropriate dosing may worsen antibiotic resistance. Dogs require veterinary-specific medications with proper dosing based on their weight and condition. Always consult a veterinarian for proper diagnosis and prescription of veterinary-approved medications that are safe and effective for canine use.
Why does my dog keep getting pyoderma despite treatment?
Recurrent pyoderma indicates an underlying cause that hasn’t been identified or properly managed, such as allergies, endocrine diseases, or immune disorders. Your veterinarian needs to investigate and treat these primary conditions through allergy testing, blood work for hormonal imbalances, or immune system evaluation to break the cycle of recurring infections.
Are certain dog breeds more prone to pyoderma?
Yes, breeds with skin folds like Bulldogs, Pugs, Shar-Pei, and Spaniels are predisposed to skin fold pyoderma due to trapped moisture and reduced air circulation. Breeds prone to allergies or endocrine diseases may develop other forms of pyoderma more frequently. Additionally, dogs with compromised immune systems or those taking certain medications face increased risk.
Can I prevent pyoderma in my dog?
While not always preventable, you can reduce risk by maintaining good hygiene, managing allergies through proper diet and environmental control, controlling parasites with regular preventive treatments, keeping skin folds clean and dry, and addressing underlying health conditions promptly with veterinary care. Regular grooming and maintaining a healthy weight also help prevent skin problems that can lead to bacterial infections.






