

Key Takeaways
Collapsing trachea causes a distinctive goose-like honking cough and occurs when cartilage rings weaken and flatten the windpipe
- Collapsing trachea causes a distinctive goose-like honking cough and occurs when cartilage rings weaken and flatten the windpipe
- Small breed dogs like Yorkshire Terriers, Chihuahuas, and Toy Poodles are most commonly affected, typically in middle age (4-14 years)
- The condition progresses through four grades from 25% to 100% tracheal narrowing, with Grade 4 requiring emergency care
- Treatment includes medical management with cough suppressants and anti-inflammatories, plus lifestyle changes like weight management and using harnesses
- Most dogs can live a normal life with proper treatment, even though the condition is progressive and requires lifelong management
Small breed dogs like Yorkshire Terriers, Chihuahuas, and Toy Poodles are most commonly affected, typically in middle age (4-14 years)
The condition progresses through four grades from 25% to 100% tracheal narrowing, with Grade 4 requiring emergency care
Treatment includes medical management with cough suppressants and anti-inflammatories, plus lifestyle changes like weight management and using harnesses
Most dogs can live a normal life with proper treatment, even though the condition is progressive and requires lifelong management
If your dog has developed a distinctive honking cough that sounds like a goose calling, you may be witnessing the hallmark sign of collapsing trachea in dogs. This progressive respiratory condition affects thousands of dogs annually, particularly small and toy breeds, but with proper understanding and management, many dogs continue to live comfortable, fulfilling lives.
Tracheal collapse represents one of the most common respiratory disorders in small breed dogs, yet it remains manageable when owners recognize the clinical signs early and work closely with their veterinarian. While the condition cannot be cured, evidence-based treatment approaches can significantly improve your dog’s quality of life and slow disease progression.
What Is Collapsing Trachea in Dogs?
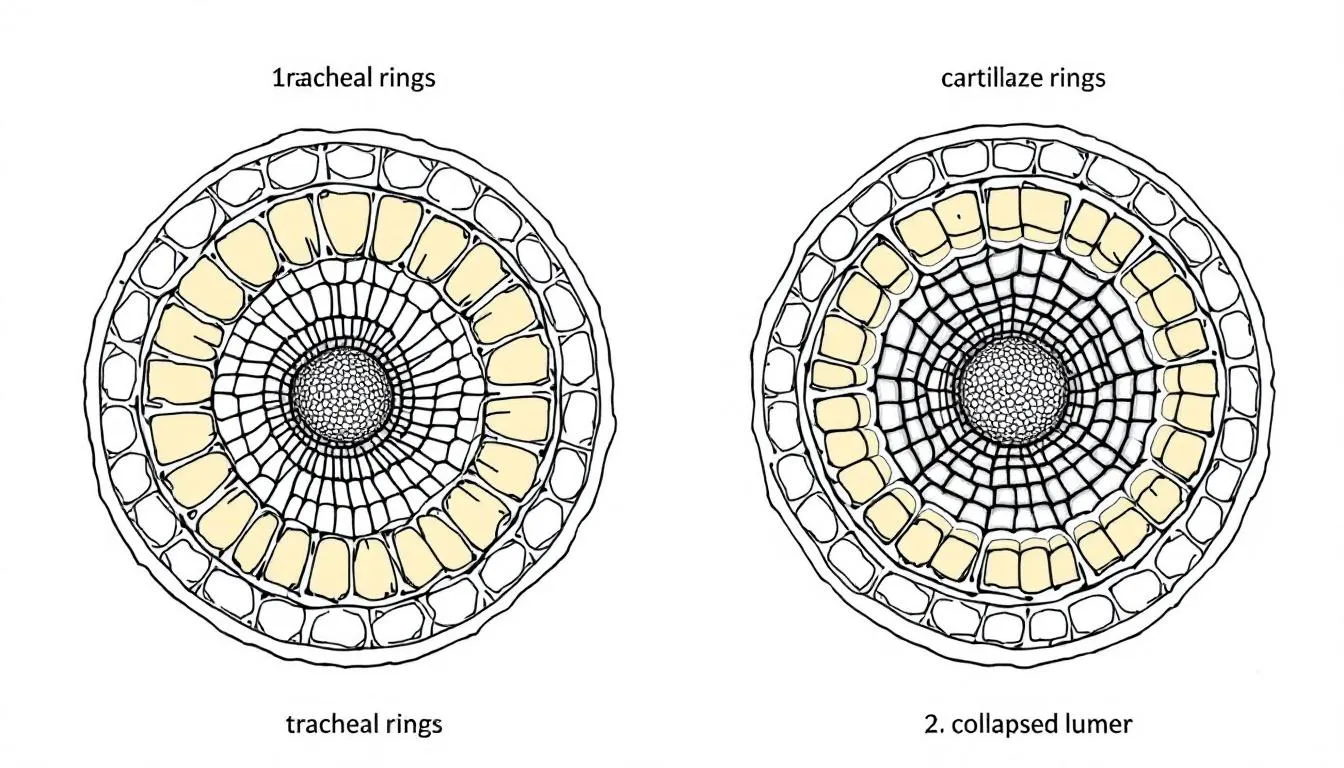
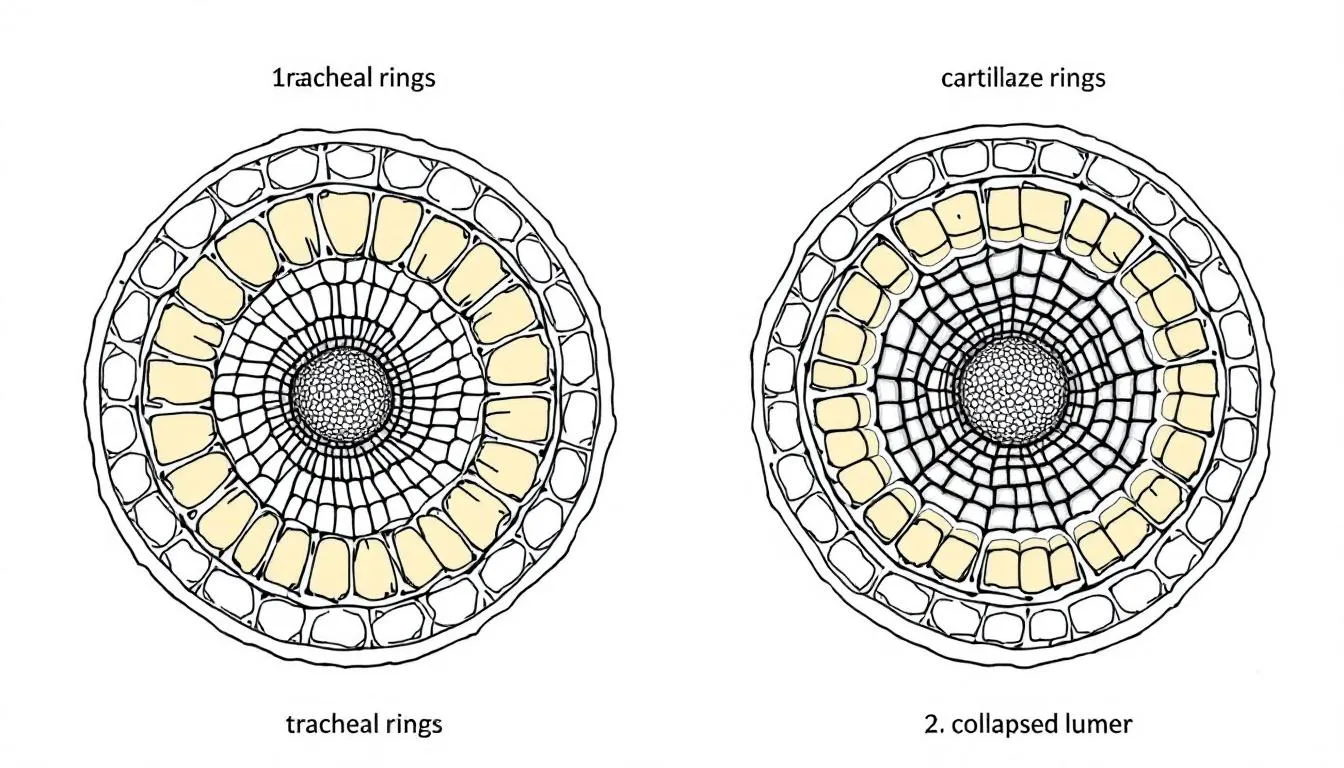
Collapsing trachea occurs when the c shaped cartilage rings that normally maintain the structural integrity of your dog’s trachea begin to weaken and flatten. The trachea, commonly known as the windpipe, serves as the vital airway connecting the nose and mouth to the lungs. In healthy dogs, these small cartilage rings keep the tracheal passage open, allowing unrestricted airflow during breathing.
When tracheal cartilage deteriorates—a process called chondromalacia—the normally rigid rings lose their ability to maintain their shape. The dorsal membrane, which forms the flexible top portion of the trachea, becomes lax and billows inward during breathing. This collapse occurs primarily when the dog inhales, creating a narrowed airway that restricts oxygen flow and triggers the characteristic symptoms. Tracheal collapse makes it difficult for air to pass through the dog's airway, resulting in labored breathing and coughing.
The condition is progressive by nature, meaning it typically worsens over time as the tracheal cartilage continues to degenerate. However, canine tracheal collapse progresses at different rates in different dogs, and many affected dogs maintain excellent quality of life for years with appropriate medical management and lifestyle modifications.
Unlike some acute respiratory conditions, tracheal collapse develops gradually, often allowing dogs and their owners time to adapt to the changing breathing patterns. This progressive disease primarily affects the respiratory system’s upper portion, though in advanced cases, it may extend to involve the bronchi—a condition termed tracheobronchomalacia.
Symptoms and Clinical Signs
The most recognizable symptom of tracheal collapse is a dry, harsh cough that distinctly resembles the honking sound of a goose. This characteristic honking cough differentiates tracheal collapse from other respiratory conditions and often prompts owners to seek veterinary care. The cough typically occurs in episodes and may be accompanied by a distinctive “snorting” sound as the dog attempts to clear the airway.
Coughing episodes are frequently triggered by specific activities or circumstances. Excitement, exercise, eating, drinking, or any gentle pressure applied to the neck area can precipitate a coughing fit. Many dogs experience their most severe symptoms during periods of high activity or stress, when increased respiratory demand exacerbates the breathing difficulty.
Additional clinical signs include retching or gagging motions, particularly following coughing episodes. Dogs may exhibit rapid breathing, even during rest periods, and show marked exercise intolerance. Many affected dogs begin to avoid activities they previously enjoyed, preferring to rest rather than engage in vigorous play. Sleep disturbances are common, as the supine position can worsen respiratory distress.
Emergency symptoms requiring immediate veterinary attention include blue-tinged gums or tongue (cyanosis), sometimes referred to as blue gums, indicating oxygen deprivation. Fainting or collapse during or following coughing episodes represents a medical emergency. Severe respiratory distress, characterized by open-mouth breathing, extended neck positioning, or inability to settle and rest, demands urgent intervention.
The dog’s symptoms often worsen during specific environmental conditions. Hot and humid environments increase respiratory effort and can trigger more frequent coughing episodes. Exposure to airborne irritants such as cigarette smoke, strong perfumes, dust, or cleaning chemicals commonly exacerbates symptoms. Many owners notice that symptoms intensify at night, possibly due to changes in breathing patterns during sleep.
Stages and Grading System
Veterinarians classify tracheal collapse using a four-grade system that helps determine appropriate treatment approaches and provides insight into prognosis. This grading system, based on the percentage of tracheal narrowing, guides medical decision-making and helps owners understand their dog’s condition severity.
Grade 1 represents the mildest form, with approximately 25% narrowing of the tracheal lumen. The cartilage rings maintain most of their normal shape, and the dorsal membrane shows only slight sagging. Dogs in this stage may exhibit occasional mild coughing, particularly during excitement or exercise, but generally maintain normal activity levels and breathing patterns.
Grade 2 involves roughly 50% narrowing, with more noticeable flattening of the tracheal rings. The dorsal membrane becomes more lax and begins to obstruct airflow more significantly. Dogs typically display intermittent coughing that becomes more frequent during triggers like exercise or excitement. Some exercise intolerance may become apparent, though most dogs continue their normal routines with minor modifications.
Grade 3 represents severe narrowing at approximately 75% of the normal tracheal diameter. The cartilage rings appear significantly flattened, and the dorsal membrane substantially intrudes into the airway. Dogs experience more frequent breathing difficulties, persistent coughing, and marked exercise intolerance. Daily activities may require modification, and symptoms often interfere with sleep quality.
Grade 4 constitutes complete or near-complete tracheal collapse, with the airway essentially closed during breathing cycles. This stage represents a medical emergency requiring immediate intervention. Dogs cannot maintain adequate oxygen levels and may experience life-threatening respiratory distress. The collapse occurs during both inspiration and expiration, severely compromising the dog’s ability to breathe effectively.
Understanding these grades helps owners recognize when their dog’s condition may be progressing and when more aggressive treatment approaches might be necessary. The grading system also assists veterinarians in determining whether medical management remains appropriate or if surgical intervention should be considered. The prognosis and management of tracheal collapse depends on the grade of collapse and the dog's response to treatment.
Causes and Risk Factors
The primary cause of tracheal collapse stems from congenital weakness in the tracheal cartilage, making this largely a genetic condition. Small breed dogs inherit a predisposition to cartilage degeneration that becomes apparent as they age. The exact genetic mechanisms remain under investigation, but the familial clustering of cases in certain bloodlines suggests a hereditary component.
Breed predisposition is remarkably strong, with toy and small breeds accounting for the vast majority of cases. Yorkshire Terriers, Pomeranians, Toy Poodles, Maltese, Chihuahuas, Pugs, and Shih Tzus are commonly affected. These breeds typically weigh less than 15 pounds, and studies suggest that up to 80% of tracheal collapse cases occur in dogs within this weight range. Lhasa Apsos and other small breeds also show increased susceptibility.
Several contributing factors can accelerate the development or worsen the symptoms of tracheal collapse. Obesity significantly increases respiratory workload and places additional stress on an already compromised airway. Excess weight forces the respiratory system to work harder, potentially hastening cartilage deterioration and intensifying symptoms in affected dogs.
Respiratory infections, whether bacterial or viral, can trigger inflammatory responses that further weaken tracheal cartilage and exacerbate collapse. Dogs with histories of chronic bronchitis or recurrent respiratory infections may be at higher risk for developing more severe forms of tracheal collapse.
Heart disease, particularly common in small breeds, can compound the effects of tracheal collapse. When the heart cannot pump efficiently, increased respiratory effort places additional strain on the compromised trachea. The combination of cardiac and respiratory compromise can create a dangerous cycle of worsening symptoms.
Environmental factors play significant roles in both symptom development and progression. Exposure to respiratory irritants including cigarette smoke, household chemicals, dust, and air pollution can trigger inflammation and worsen cartilage degeneration. Even seemingly innocuous substances like air fresheners or cleaning products can serve as triggers for sensitive dogs.
Age represents another important factor, with tracheal collapse most commonly diagnosed in middle aged and older dogs. Most dogs develop clinical signs between 4 and 14 years of age. The mean age at diagnosis typically falls around 6-7 years, though younger dogs with severe congenital weakness may show symptoms earlier, while others may not develop noticeable signs until their senior years.


Diagnosis and Testing
Diagnosing tracheal collapse requires a comprehensive approach combining clinical assessment, imaging studies, and sometimes direct visualization of the airway. The diagnostic process typically begins with a thorough history and physical exam, where veterinarians gather crucial information about the onset, progression, and triggers of your dog’s symptoms.
During the initial assessment, your veterinarian will carefully listen to your dog’s breathing patterns and may attempt to trigger a coughing episode by applying gentle pressure to the tracheal area. Many veterinarians appreciate when owners bring videos of coughing episodes, as these episodes may not occur during the examination but provide valuable diagnostic information.
Veterinarians use imaging and endoscopy to examine the dog's body and internal structures, which is essential for diagnosing conditions like trachea collapse. Standard chest and neck radiographs (X-rays) serve as important screening tools, though they may not always reveal the full extent of tracheal collapse. X-rays can show the static appearance of the trachea and help rule out other respiratory conditions, but they may miss dynamic collapse that occurs only during breathing. Studies suggest that up to 40% of dogs with tracheal collapse may have normal-appearing X-rays when the images are taken during quiet breathing.
Fluoroscopy provides superior diagnostic information by allowing real-time observation of tracheal movement during breathing cycles. This dynamic imaging technique can capture the collapse as it occurs during inspiration and expiration, providing crucial information about the location and severity of the problem. Fluoroscopy helps determine whether the collapse affects the cervical (neck) portion, thoracic (chest) portion, or both areas of the trachea.
For definitive diagnosis and grading, many veterinarians recommend bronchoscopy or endoscopy. This procedure involves inserting a small camera into the airway to directly visualize the tracheal collapse and assess its severity. Bronchoscopy represents the gold standard for diagnosis, allowing veterinarians to accurately grade the collapse and identify any concurrent bronchial involvement.
Additional diagnostic tests may include blood work to assess overall health and rule out concurrent conditions. Echocardiograms may be recommended to evaluate heart function, particularly important given the high incidence of heart disease in small breed dogs. These tests help veterinarians develop comprehensive treatment plans that address all aspects of your dog’s health.
Treatment Options
Treatment for tracheal collapse focuses on managing symptoms, slowing progression, and maintaining quality of life, as the cartilage degeneration cannot be reversed. The primary goal of treatment is to improve the dog's quality of life by addressing symptoms and supporting overall well-being. The approach varies significantly based on the severity of collapse, concurrent health conditions, and individual patient factors. Most dogs benefit from medical management, while surgical intervention is reserved for severe cases that don’t respond adequately to conservative treatment.
The treatment strategy typically involves a multi-modal approach addressing the primary respiratory symptoms while managing contributing factors like obesity, environmental triggers, and concurrent diseases. Success depends heavily on early intervention, consistent management, and regular monitoring to adjust treatments as the condition progresses.
Veterinary internal medicine specialists often lead the treatment team for complex cases, coordinating care between multiple disciplines to optimize outcomes. The goal is not cure, but rather long-term management that allows dogs to maintain comfortable, active lives despite their progressive disease.
Medical Management
Medical treatment forms the cornerstone of tracheal collapse management for most affected dogs. Cough suppressants represent the primary therapeutic intervention, helping reduce the irritation and trauma caused by persistent coughing. Commonly prescribed medications include butorphanol and hydrocodone, which effectively suppress the cough reflex while allowing dogs to maintain adequate respiratory function.
Anti-inflammatory medications play crucial roles in reducing tracheal swelling and irritation. Oral corticosteroids like prednisolone are frequently prescribed during acute exacerbations, while inhaled steroids may provide long-term anti-inflammatory benefits with fewer systemic side effects. These medications help decrease inflammation within the airway, potentially reducing the severity of collapse episodes.
Bronchodilators may be beneficial for some dogs, particularly those with concurrent small airway disease. These medications help widen the airways and reduce resistance to airflow, though their effectiveness in tracheal collapse specifically remains somewhat controversial. Some dogs show marked improvement with bronchodilator therapy, while others experience minimal benefit.
When secondary bacterial infections complicate tracheal collapse, antibiotics become necessary components of the treatment plan. However, antibiotics should only be used when bacterial infection is confirmed, as inappropriate antibiotic use can contribute to resistance and doesn’t address the underlying cartilage problem.
Sedatives may be prescribed for dogs whose coughing episodes are triggered by excitement or anxiety. By reducing the dog’s stress response and excitement level, these medications can help prevent the triggering events that lead to severe coughing fits and respiratory distress.
Management of concurrent conditions represents an essential aspect of medical treatment. Dogs with heart disease require cardiac medications to optimize heart function and reduce the strain on the respiratory system. Similarly, treatment of chronic bronchitis or other respiratory conditions helps minimize the overall burden on the compromised airway.
It is important to closely monitor the dog's response to medical management and adjust treatment as needed to achieve the best possible outcome.
Surgical Options
Surgical intervention becomes necessary when medical management fails to adequately control symptoms or when dogs develop life-threatening respiratory distress. Surgical procedures are often considered for dogs with severely collapsed tracheas that do not respond to medical management, as these interventions can help stabilize the airway and improve quality of life. The decision to pursue surgical treatment requires careful consideration of the dog’s overall health, the location and severity of collapse, and the owner’s commitment to post-operative care.
Intraluminal tracheal stent placement represents the most commonly performed surgical procedure for severe tracheal collapse. During this procedure, a board certified veterinary surgeon places a tubular mesh device (stent) inside the collapsed portion of the trachea to maintain airway patency. These stents are typically made of materials like nitinol, a memory metal that expands to predetermined dimensions once deployed.
The surgical procedure involves general anesthesia and endoscopic guidance to precisely position the stent within the collapsed tracheal segment. Success rates for immediate improvement in airway patency exceed 80%, with most dogs experiencing dramatic improvement in breathing effort and reduction in cyanotic episodes.
External prosthetic ring placement offers an alternative surgical approach, though it’s less commonly used in modern practice. This technique involves surgically placing C-shaped rings around the outside of the trachea to provide structural support. While effective for cervical tracheal collapse, this approach is less suitable for thoracic collapse and carries higher surgical risks.
Potential surgical complications include stent migration, where the device moves from its intended position, potentially causing new obstruction. Granulation tissue formation can occur around stents, requiring additional procedures to remove excess tissue growth. Infection represents another risk, particularly in the immediate post-operative period.
Post-surgical care requires continued medical management, as surgery addresses the mechanical obstruction but doesn’t eliminate the underlying disease process. Many dogs continue to cough after stent placement due to mechanical irritation from the device, though the intensity typically decreases significantly compared to pre-surgical symptoms.
Long-term outcomes vary, with median survival times ranging from 1-4 years post-stenting, depending on the severity of disease, concurrent conditions, and the dog’s response to ongoing medical management. While surgery can be life-saving for dogs with severe collapse, it’s important to understand that it represents palliative rather than curative treatment.
Oxygen Therapy
Oxygen therapy plays a vital role in supporting dogs with tracheal collapse, especially during episodes of respiratory distress when the airway becomes severely narrowed. By delivering concentrated oxygen, this therapy helps increase the amount of oxygen available to your dog’s body, easing the burden on the compromised respiratory system and helping to prevent dangerous drops in blood oxygen levels.
Veterinarians may administer oxygen therapy in several ways, depending on your dog’s needs and the severity of their symptoms. Common methods include oxygen masks, nasal tubes, or specialized oxygen cages that create a controlled environment for your dog to breathe more easily. In emergency situations, oxygen therapy can provide immediate relief and stabilize your dog while further treatment is planned.
Ongoing oxygen therapy may be recommended for dogs with advanced tracheal collapse or those recovering from a severe episode. Your veterinarian will determine the most appropriate method and duration of therapy, and may teach you how to recognize signs that your dog needs supplemental oxygen at home. Regular monitoring and adjustments ensure that your dog receives the right level of support, helping to manage tracheal collapse and reduce the risk of complications related to oxygen deprivation.
Managing Coughing Episodes
Coughing episodes are a hallmark of tracheal collapse in dogs and can be distressing for both pets and their owners. Effectively managing these episodes is key to minimizing irritation and preventing further damage to the trachea. One of the most important steps is to keep your dog calm and relaxed, as excitement, anxiety, or vigorous activity can trigger or worsen coughing fits.
Avoiding known triggers—such as pulling on the leash, exposure to smoke or dust, or overexertion—can help reduce the frequency and severity of coughing episodes. Using a harness instead of a collar is especially important to prevent pressure on the trachea during walks. Your veterinarian may prescribe cough suppressants to help control persistent coughing and break the cycle of irritation. In some cases, anti-inflammatory medications or bronchodilators may also be recommended to decrease airway inflammation and make breathing easier.
It’s important to monitor your dog’s coughing episodes closely. If you notice that the episodes are becoming more frequent, severe, or are accompanied by other symptoms like difficulty breathing or blue-tinged gums, seek veterinary care promptly. Early intervention can help prevent complications and keep your dog comfortable.


Management and Lifestyle Changes
Effective management of tracheal collapse extends far beyond medical treatment, encompassing comprehensive lifestyle modifications that can dramatically improve your dog’s quality of life. Weight management stands as perhaps the most crucial factor, with studies showing that weight loss can improve symptoms in up to 70% of overweight dogs with tracheal collapse.
Maintaining a healthy weight reduces the respiratory workload and decreases pressure on the compromised trachea. Even modest weight reductions can yield significant improvements in breathing comfort and exercise tolerance. Working with your veterinarian to develop a safe, gradual weight loss plan ensures that your dog loses weight without compromising nutritional needs or overall health.
Exercise modification becomes essential for dogs with tracheal collapse, though complete exercise restriction is rarely necessary or beneficial. The key lies in adjusting activities to match your dog’s capabilities while avoiding triggers that precipitate severe coughing episodes. Short, controlled walks on flat terrain often work better than vigorous play sessions or activities requiring sustained exertion.
Swimming can provide excellent low-impact exercise for dogs who enjoy water activities, as the buoyancy reduces stress on the respiratory system while maintaining cardiovascular fitness. However, care must be taken to ensure the dog doesn’t become overly excited, which could trigger coughing episodes even in the water.
Environmental management plays a vital role in symptom control. Avoiding airway irritants such as cigarette smoke, strong perfumes, household cleaners, and dusty environments can significantly reduce coughing episodes. Air purifiers and regular cleaning can help maintain better indoor air quality, while avoiding outdoor activities during high pollution days protects sensitive airways.
Humidity control in the home environment can also impact symptoms. Very dry air can irritate already sensitive airways, while excessive humidity may worsen breathing difficulties in some dogs. Maintaining moderate humidity levels and ensuring good air circulation helps create optimal breathing conditions.
Equipment changes, particularly switching from collars to harnesses, can prevent pressure on the neck area that might trigger coughing episodes. A properly fitted harness distributes pressure across the chest rather than concentrating it on the tracheal area, allowing for more comfortable walks and reducing the risk of triggering collapse episodes.
Stress reduction techniques benefit many dogs with tracheal collapse, as anxiety and excitement can precipitate severe symptoms. Maintaining calm environments during coughing episodes, avoiding overstimulation, and using calming techniques can help minimize symptom frequency and severity.
Preventing Complications
Preventing complications is a crucial part of managing tracheal collapse in dogs and ensuring the best possible quality of life. One of the most effective strategies is maintaining your dog at a healthy weight, as excess weight puts additional strain on the respiratory system and can worsen breathing difficulties. Work with your veterinarian to develop a safe weight management plan if needed.
Minimizing exposure to airway irritants is equally important. Avoid cigarette smoke, strong cleaning products, dust, and other environmental triggers that can inflame the trachea and provoke coughing or respiratory distress. Keeping your home well-ventilated and using air purifiers can help create a safer environment for your dog.
Regular veterinary check-ups are essential for early detection of potential complications, such as infections or worsening collapse. Be vigilant for warning signs like rapid breathing, blue tinged gums, or increased difficulty breathing, and seek immediate veterinary care if these occur. By taking proactive steps and staying alert to changes in your dog’s condition, you can help prevent serious complications and support your dog’s respiratory health.
Prognosis and Long-term Outlook
The prognosis for dogs with tracheal collapse varies significantly based on several factors, but many dogs live normal lifespans with appropriate management. Early diagnosis and prompt implementation of medical treatment and lifestyle modifications generally result in better long-term outcomes than delayed intervention after severe symptoms have developed.
Most dogs with mild to moderate tracheal collapse (Grades 1-2) maintain excellent quality of life for years following diagnosis. These dogs typically respond well to medical management and lifestyle changes, often requiring only minor adjustments to their daily routines. With proper care, many continue to enjoy walks, play sessions, and normal interactions with their families.
Dogs with more severe collapse (Grade 3) may experience more significant lifestyle limitations but can still maintain good quality of life with careful management. These dogs often require more intensive medical treatment and closer monitoring, but many continue to enjoy comfortable lives for several years following diagnosis.
The progressive nature of tracheal collapse means that symptoms typically worsen over time, though the rate of progression varies considerably between individual dogs. Some dogs experience rapid deterioration over months, while others maintain stable symptoms for years. Regular veterinary monitoring allows for treatment adjustments as the condition evolves.
Concurrent conditions significantly impact prognosis. Dogs with heart disease, chronic bronchitis, or severe obesity generally have more guarded prognoses than those with isolated tracheal collapse. However, aggressive management of these concurrent conditions can substantially improve outcomes even in complex cases.
For dogs requiring surgical intervention, prognosis depends on multiple factors including the location of collapse, overall health status, and response to post-operative care. While tracheal stent placement can provide dramatic short-term improvement, the long-term outlook requires continued medical management and monitoring for potential complications.
Quality of life considerations become paramount in long-term management decisions. Regular assessment of the dog’s comfort level, activity tolerance, and overall enjoyment of life helps guide treatment intensification or, in some cases, difficult end-of-life decisions. Most dogs with tracheal collapse maintain good quality of life throughout most of their disease course with appropriate care.
Studies suggest that approximately 75% of dogs treated medically survive at least two years following diagnosis, with many living much longer. The key to optimal outcomes lies in early recognition, prompt treatment, and consistent long-term management tailored to each individual dog’s needs and response.


When to Seek Emergency Care
Recognizing when tracheal collapse symptoms require immediate veterinary attention can be life-saving for your dog. While many symptoms of tracheal collapse develop gradually and can be managed on an outpatient basis, certain signs indicate severe respiratory compromise requiring urgent intervention.
Blue or purple gums represent a medical emergency indicating inadequate oxygen levels in the blood. This cyanosis signals that the airway obstruction has become severe enough to prevent adequate oxygenation, requiring immediate veterinary attention and potentially supplemental oxygen therapy. Any color change in the gums or tongue from normal pink to blue, purple, or gray warrants emergency care.
Severe respiratory distress characterized by open-mouth breathing, extended head and neck positioning, or visible struggle to breathe indicates critical airway compromise. Dogs exhibiting these signs cannot maintain adequate ventilation and require urgent medical intervention, possibly including sedation, oxygen therapy, or emergency procedures to establish airway patency.
Fainting or collapse episodes during or following coughing fits represent serious complications that may indicate inadequate brain oxygenation. These episodes, known as syncope, can result from severe airway obstruction or secondary cardiac effects and require immediate evaluation and treatment.
Inability to settle or rest due to continuous coughing and labored breathing indicates that the dog’s respiratory system is severely compromised. Dogs who cannot lie down comfortably or who must maintain upright positions to breathe effectively need urgent veterinary assessment and intervention.
Prolonged coughing episodes that don’t resolve with typical interventions may progress to severe respiratory distress. If coughing fits last more than several minutes or if the dog appears to be choking or cannot catch their breath between coughs, emergency care is warranted.
While waiting for emergency veterinary care, owners can take several steps to help their dog. Moving to a cool, well-ventilated area with clean air can help reduce respiratory distress. Keeping the dog calm and avoiding excitement or stress can prevent worsening of symptoms. However, these measures are temporary, and professional veterinary intervention remains essential for dogs experiencing severe symptoms.
Having an emergency plan in place before crisis situations arise helps ensure rapid response when every minute counts. Knowing the location of the nearest 24-hour veterinary facility and having contact information readily available can save valuable time during emergency situations.
Working with a Veterinarian
A strong partnership with your veterinarian is essential for successfully managing tracheal collapse in dogs. Your veterinarian will help diagnose tracheal collapse through a combination of physical exams, imaging, and possibly advanced diagnostics, ensuring an accurate understanding of your dog’s condition. Together, you’ll develop a tailored treatment plan that may include medical management, lifestyle adjustments, and, in severe cases, surgical intervention.
Regular veterinary visits allow for ongoing monitoring of your dog’s symptoms and timely adjustments to their treatment plan. If your dog’s condition progresses or does not respond to standard therapies, your veterinarian may refer you to a board certified veterinary surgeon for advanced procedures such as tracheal stent placement. These specialists have the expertise to perform surgical interventions that can provide relief in severe cases of tracheal collapse.
By working closely with your veterinary team, you can ensure that your dog receives comprehensive care, from routine check-ups to specialized treatments. Open communication and prompt attention to changes in your dog’s symptoms will help maintain their quality of life and manage the challenges of tracheal collapse effectively.
FAQ
Can collapsing trachea be prevented in dogs?
Currently, there is no known way to prevent tracheal collapse due to its genetic nature, but maintaining healthy weight and avoiding respiratory irritants may help reduce symptom severity in predisposed dogs. Since the condition stems from inherited cartilage weakness, breeding programs that screen for affected lines may help reduce incidence over time, though genetic testing is not yet widely available.
What is the best sleeping position for dogs with collapsing trachea?
Dogs with collapsing trachea sleep best on their sides with their head and neck slightly elevated using bolster beds or pillows, which helps keep airways open and reduces pressure on the trachea during rest. Some dogs prefer sleeping in a slightly upright position against cushions or in elevated beds that allow gravity to help maintain airway patency.
How can I tell the difference between collapsing trachea and other respiratory conditions?
Collapsing trachea produces a distinctive dry, honking cough that sounds like a goose, typically triggered by excitement or pressure on the neck, unlike wet productive coughs from infections or heart-related coughs that may occur with fluid retention. The timing and triggers of the cough, along with the characteristic sound quality, help differentiate tracheal collapse from other respiratory conditions, though veterinary evaluation is necessary for definitive diagnosis.
Is surgery always necessary for severe tracheal collapse?
Surgery is not always necessary and is typically reserved for dogs whose symptoms cannot be controlled with medications and lifestyle changes; many dogs with even Grade 3 collapse can be managed successfully without surgical intervention. The decision for surgery depends on the dog’s response to medical management, quality of life, overall health status, and the specific location and characteristics of the collapse.
Can collapsing trachea symptoms get worse with age?
Yes, tracheal collapse is a progressive condition that typically worsens over time as cartilage continues to weaken, but proper management can slow progression and maintain quality of life for many years. The rate of progression varies significantly between individual dogs, with some experiencing gradual changes over years while others may have more rapid deterioration, making regular veterinary monitoring essential for optimal management.
FAQ
Can collapsing trachea be prevented in dogs?
Currently, there is no known way to prevent tracheal collapse due to its genetic nature, but maintaining healthy weight and avoiding respiratory irritants may help reduce symptom severity in predisposed dogs. Since the condition stems from inherited cartilage weakness, breeding programs that screen for affected lines may help reduce incidence over time, though genetic testing is not yet widely available.
What is the best sleeping position for dogs with collapsing trachea?
Dogs with collapsing trachea sleep best on their sides with their head and neck slightly elevated using bolster beds or pillows, which helps keep airways open and reduces pressure on the trachea during rest. Some dogs prefer sleeping in a slightly upright position against cushions or in elevated beds that allow gravity to help maintain airway patency.
How can I tell the difference between collapsing trachea and other respiratory conditions?
Collapsing trachea produces a distinctive dry, honking cough that sounds like a goose, typically triggered by excitement or pressure on the neck, unlike wet productive coughs from infections or heart-related coughs that may occur with fluid retention. The timing and triggers of the cough, along with the characteristic sound quality, help differentiate tracheal collapse from other respiratory conditions, though veterinary evaluation is necessary for definitive diagnosis.
Is surgery always necessary for severe tracheal collapse?
Surgery is not always necessary and is typically reserved for dogs whose symptoms cannot be controlled with medications and lifestyle changes; many dogs with even Grade 3 collapse can be managed successfully without surgical intervention. The decision for surgery depends on the dog’s response to medical management, quality of life, overall health status, and the specific location and characteristics of the collapse.
Can collapsing trachea symptoms get worse with age?
Yes, tracheal collapse is a progressive condition that typically worsens over time as cartilage continues to weaken, but proper management can slow progression and maintain quality of life for many years. The rate of progression varies significantly between individual dogs, with some experiencing gradual changes over years while others may have more rapid deterioration, making regular veterinary monitoring essential for optimal management.






