Key Takeaways
- Colitis is inflammation of the large intestine (colon) causing bloody diarrhea, mucus in stool, and frequent urges to defecate
- Acute colitis often resolves within 3-5 days with dietary changes and basic treatment, while chronic colitis requires extensive veterinary evaluation
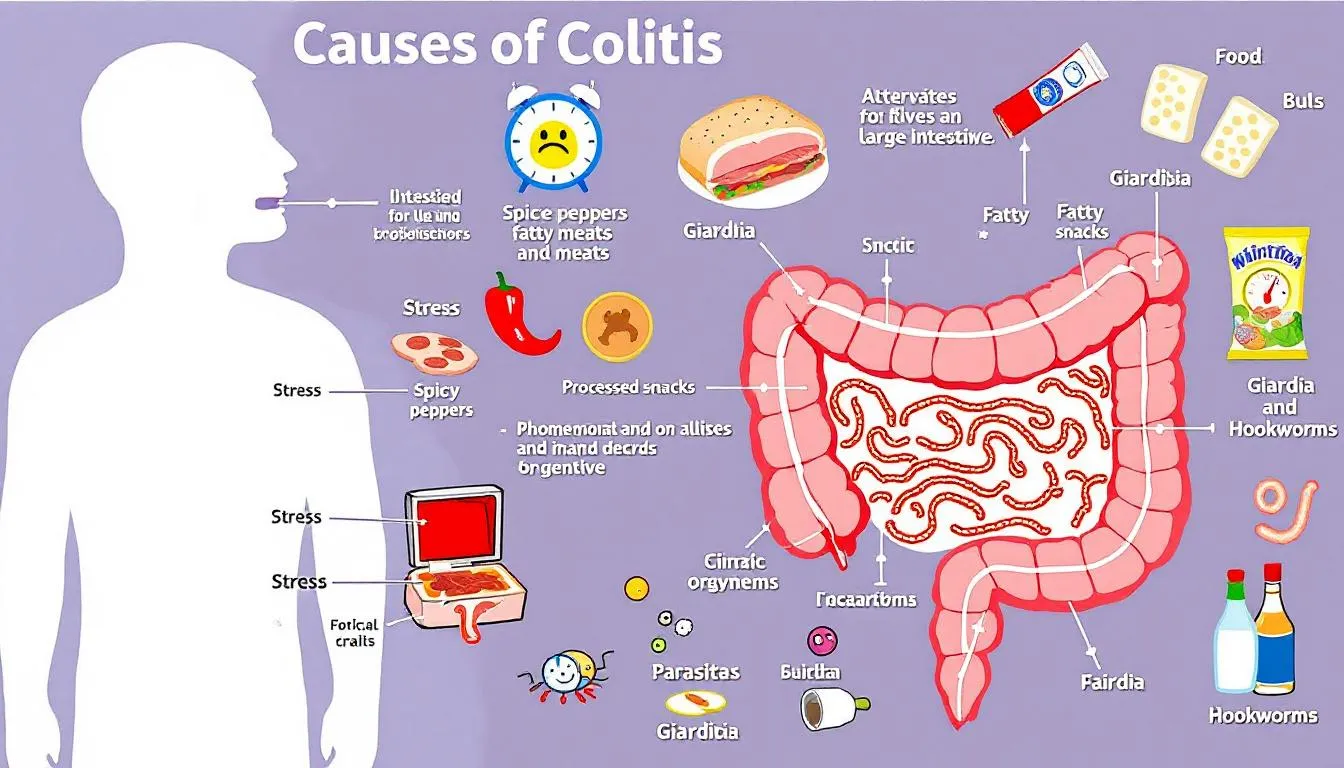
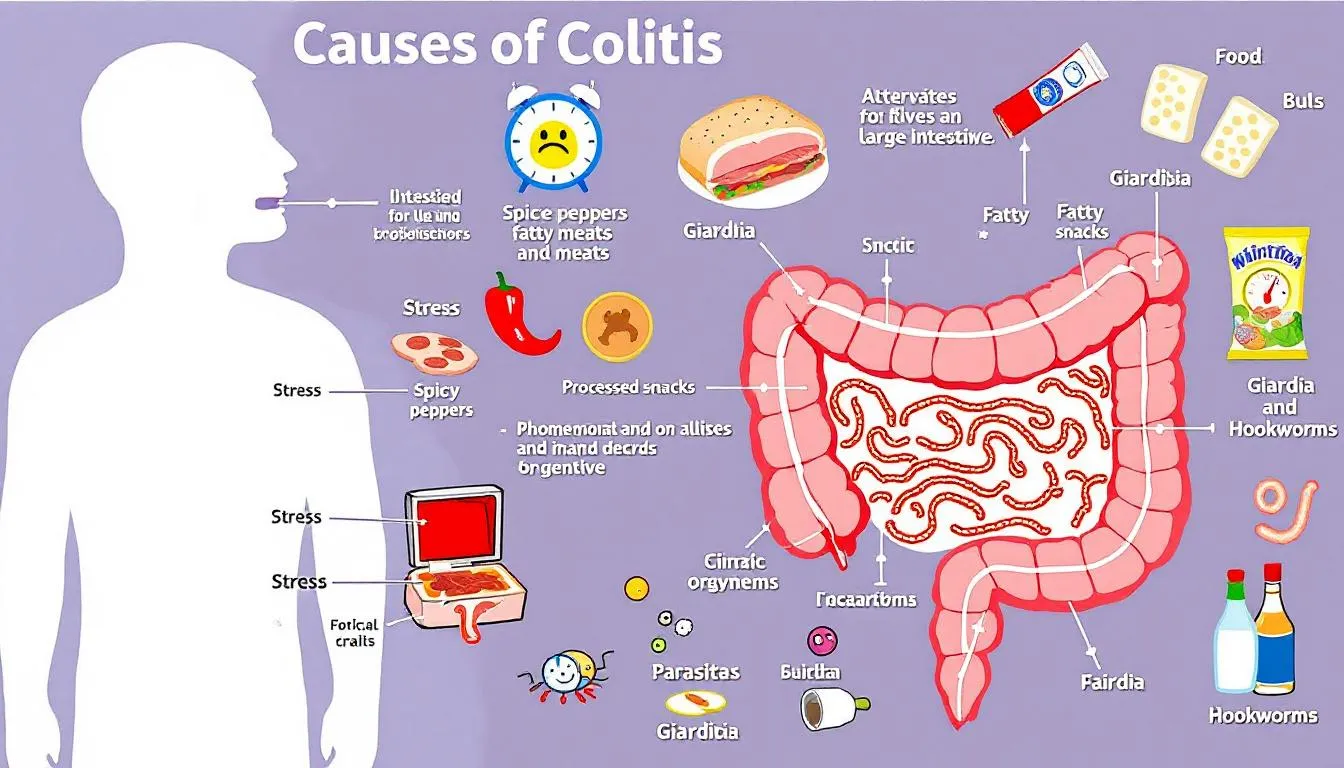
- Common causes include stress, dietary indiscretion, parasites like whipworms and giardia, bacterial infections, and food allergies
- Treatment involves antibiotics like metronidazole, dietary fiber supplements, bland diets, and prescription hypoallergenic foods
- Most dogs recover completely from acute colitis, but chronic cases need ongoing management with specialized diets and medications
Colitis is inflammation of the large intestine (colon) causing bloody diarrhea, mucus in stool, and frequent urges to defecate
Acute colitis often resolves within 3-5 days with dietary changes and basic treatment, while chronic colitis requires extensive veterinary evaluation
Common causes include stress, dietary indiscretion, parasites like whipworms and giardia, bacterial infections, and food allergies
Treatment involves antibiotics like metronidazole, dietary fiber supplements, bland diets, and prescription hypoallergenic foods
Most dogs recover completely from acute colitis, but chronic cases need ongoing management with specialized diets and medications


What is Colitis in Dogs?
Colitis in dogs is defined as inflammation of the large intestine, also called colitis, which disrupts normal digestive function and causes significant discomfort. The dog’s colon normally absorbs water from waste material and houses beneficial bacteria that support gut health. The dog's colon is essential for digestion and water absorption; when inflammation affects the dog's colon, its ability to perform these functions is impaired, often resulting in diarrhea and cramping. When inflammation occurs, this delicate balance is disrupted, leading to the characteristic symptoms pet owners recognize.
The large intestine plays a crucial role in processing waste with beneficial bacteria working to maintain proper digestive function. During colitis, inflammatory cells infiltrate the colon wall, reducing its ability to absorb water effectively. This process results in loose stools containing bright red blood and mucus, distinguishing large bowel diarrhea from small intestinal diarrhea.
Understanding the difference between large bowel and small intestinal diarrhea helps identify when colitis may be present. Large intestinal diarrhea typically involves frequent, small-volume stools with blood and mucus, while small intestinal diarrhea usually produces larger volumes of watery stool without visible blood. Weight loss is uncommon in pure large bowel disease, making this distinction clinically important.
Types of Colitis in Dogs
Acute colitis represents sudden onset inflammation lasting less than two weeks. Most dogs with acute colitis recover quickly with appropriate treatment, often within only a few days. Stress colitis, a common form of acute colitis, frequently triggers colitis symptoms following environmental changes like boarding or moving.
Chronic colitis involves persistent symptoms lasting more than two weeks, requiring comprehensive medical workup to identify underlying causes. These chronic cases often involve immune system disorders or food allergies that need long-term management strategies.
Inflammatory bowel disease represents a specific type of chronic colitis where the dog’s immune system inappropriately attacks the intestinal tract. This condition, commonly called colitis by veterinarians, requires ongoing treatment with anti inflammatory medications and specialized diets.
Stress colitis occurs when stressful events trigger acute inflammation in otherwise healthy dogs. Environmental factors like travel, boarding, or household changes can triggers colitis symptoms that typically resolve once the stressor is removed.


Symptoms and Clinical Signs of Colitis
The most recognizable symptoms of colitis include frequent attempts to defecate with small-volume production. Dogs typically show dog straining during bowel movements, producing loose stools containing fresh blood and mucus. Pet owners often notice their dog’s stool has a distinctly different appearance, with visible bright red blood coating the surface. Examining the dog's stool is important for assessing gastrointestinal issues and can provide valuable clues to the presence and severity of colitis.
Pet’s clinical signs typically include urgency to defecate, leading to indoor accidents even in well-trained dogs. The frequent urges result from inflammation irritating the colon lining, creating a sensation of incomplete evacuation. Unlike conditions affecting the small intestine, weight loss and vomiting are uncommon with pure large bowel disease.
Most dogs with colitis maintain normal appetite and energy levels between episodes, particularly in acute cases. The inflammation primarily affects stool consistency and frequency rather than overall systemic health, though severe cases may show signs of discomfort or pain.
Acute vs Chronic Colitis Symptoms
Acute colitis typically presents with sudden onset of watery diarrhea containing blood and mucus. Dogs may need to go outside multiple times per hour, and accidents in the house become common despite previous house training. These symptoms usually develop rapidly over 24-48 hours.
Chronic colitis symptoms tend to be more subtle but persistent. Dogs may have ongoing soft stools with intermittent blood or mucus, and owners might notice gradual changes in bowel movement patterns over weeks to months. The chronic cases often show periods of improvement followed by flare up episodes.
Both acute and chronic forms involve inflammation of the dog’s colon, but their duration and intensity differ significantly. Acute cases often resolve with basic treatment, while chronic enteropathies require extensive diagnostic testing and long-term management plans.
Causes of Colitis in Dogs
Multiple factors can triggers colitis in dogs, with stress-related causes being among the most common. Stressful events like boarding, traveling, moving homes, or introducing new pets can disrupt normal gut function and lead to acute inflammation. The stress response affects both immune function and intestinal motility, making the colon more susceptible to irritation.
Dietary indiscretions frequently cause colitis symptoms when dogs consume inappropriate items. Eating garbage, spoiled food, sudden diet changes, or receiving inappropriate treats can irritate the colon lining. Even well-intentioned dietary changes made too rapidly can trigger inflammatory responses in sensitive dogs. Changes in a dog's diet, or feeding a diet that does not suit the dog's digestive system, can also contribute to the development of colitis by upsetting the balance of the gastrointestinal tract.
Parasitic infections represent another major cause, with organisms like whipworms, giardia, coccidia, and cryptosporidium commonly affecting the large bowel. These parasites damage the colon lining directly, causing inflammation and characteristic bloody diarrhea. Regular parasite prevention helps reduce risk, but exposure can still occur through contaminated environments.
Bacterial infection from pathogenic bacteria like Salmonella, Clostridium perfringens, and gram negative bacteria can also cause acute colitis. These infections may result from consuming contaminated food or water, or from overgrowth of harmful bacteria when beneficial bacteria populations are disrupted.
Food allergy represents a significant cause of chronic colitis, particularly in dogs with ongoing digestive issues. Proteins from beef, chicken, dairy, or grain sources can trigger immune responses leading to persistent inflammation. Identifying specific allergens requires careful diet trial protocols lasting 8-10 weeks.
Breed Predispositions
Young Boxers and French Bulldogs show particular susceptibility to granulomatous colitis, also known as histiocytic ulcerative colitis. This severe form causes thickened bowel walls, persistent bloody diarrhea, and often leads to weight loss unlike typical large bowel disease. The condition appears linked to invasive gram negative bacteria requiring specific antibiotic treatment.
While any dog breed can develop colitis, certain genetic predispositions exist. Early recognition in predisposed breeds allows for faster diagnosis and more targeted treatment approaches. Veterinary internal medicine specialists often see these breed-specific patterns in their practice.
Most dogs of any breed can develop stress-related or dietary-induced colitis, making prevention strategies important regardless of genetic background. However, owners of predisposed breeds should be particularly alert to early symptoms and seek prompt veterinary evaluation when clinical signs appear.
Diagnosis of Colitis in Dogs
Diagnosing colitis begins with obtaining a detailed medical history focusing on symptom onset, stool appearance, recent dietary changes, and potential stress triggers. Veterinarians need information about the exact cause of symptoms, including timing relative to environmental changes or dietary indiscretions.
The thorough physical exam includes rectal evaluation to assess stool quality and check for pain or abnormalities. This examination helps differentiate large bowel from small bowel disease and may reveal evidence of parasites or foreign material.
Fresh fecal sample analysis represents the most important initial diagnostic test. Veterinarians examine samples for parasites, abnormal bacteria, and inflammatory cells. This protected culture technique helps identify specific pathogens requiring targeted treatment.
Blood tests evaluate overall health and rule out systemic diseases that might contribute to digestive symptoms. While most cases of simple colitis don’t cause significant changes in blood parameters, these tests help identify dogs needing more intensive treatment.
Advanced Diagnostic Tests
When initial treatments fail or chronic symptoms persist, additional testing becomes necessary. Fecal PCR testing can detect difficult-to-find parasites and identify specific bacterial strains that standard microscopy might miss.
Abdominal ultrasound allows veterinarians to evaluate intestinal wall thickness and check for lymph node enlargement. Thickened colon walls or enlarged lymph nodes suggest more serious underlying conditions requiring specific treatment approaches.
Colonoscopy with biopsies under general anesthesia provides definitive diagnosis for chronic cases. This procedure allows direct visualization of the colon lining and collection of tissue samples for microscopic examination. The results help distinguish inflammatory bowel disease from other chronic enteropathies.
Diet trials using novel or hydrolyzed protein diets serve as both diagnostic and therapeutic tools. These controlled feeding trials lasting 8-10 weeks help identify food allergies contributing to chronic symptoms. Success with elimination diets confirms food sensitivity as a contributing factor.
Treatment Options for Colitis
Effective treatment for colitis depends on identifying and addressing underlying causes while providing symptomatic relief. How colitis is treated depends on whether it is acute or chronic; acute colitis treated with targeted, condition-specific therapies may involve dietary management and short-term medication, while chronic colitis treated often requires advanced diagnostics, long-term medication, and emerging therapies such as fecal transplants to ensure the most effective outcome. Never give human medications to dogs with digestive issues, as many can be toxic and worsen symptoms. Immediate veterinary care becomes essential when colitis symptoms appear, particularly in puppies, elderly dogs, or those with other medical conditions.
Treatment approaches vary based on whether the condition is acute or chronic, with combination therapy often proving most effective. Veterinarians typically start with conservative management for acute cases while pursuing more aggressive diagnostic testing for chronic situations.
The goal of treatment extends beyond symptom control to address underlying causes and prevent recurrence. This comprehensive approach helps ensure long-term success and reduces the likelihood of chronic colitis development.
Medications for Colitis
Metronidazole serves as a first-line antibiotic treatment, offering both antimicrobial and anti inflammatory effects specifically beneficial for colitis. This medication targets anaerobic bacteria while reducing inflammation in the colon lining. Most dogs show improvement within 24-48 hours of starting treatment.
Tylosin provides another effective antibiotic option, particularly useful against gram-positive bacteria commonly associated with colitis. This medication concentrates in the intestinal tract, providing targeted therapy with minimal systemic effects.
Sulfasalazine delivers anti inflammatory effects directly to the large intestine, making it particularly useful for chronic inflammatory conditions. The medication breaks down in the colon to release active compounds that reduce inflammation locally.
Glucocorticoids like prednisone become necessary for dogs with confirmed inflammatory bowel disease or severe chronic colitis. These powerful anti inflammatory medications suppress immune system activity but require careful monitoring for side effects.
Enrofloxacin represents a specialized treatment specifically for histiocytic ulcerative colitis in Boxers and related breeds. This fluoroquinolone antibiotic targets the invasive bacteria associated with this severe form of granulomatous colitis.
Dietary Management
A bland diet forms the foundation of dietary treatment, typically consisting of boiled chicken, white rice, and plain canned pumpkin for dietary fiber. Veterinarians often recommend feeding dogs with colitis easily digestible foods, limited ingredient diets, or adding probiotics to support recovery and manage symptoms. This combination provides easily digestible nutrients while the added fiber helps normalize stool consistency and supports gut health.
Prescription hypoallergenic diets become necessary for dogs with suspected food allergies. A special diet is often a primary treatment option for colitis and other gastrointestinal conditions, helping to manage symptoms and promote gut healing. These specialized protein diets contain novel proteins or hydrolyzed proteins that are less likely to trigger immune responses. Strict adherence to these diets is essential for success.
High-fiber diets help improve stool consistency and support beneficial bacteria in the colon. Soluble fiber sources like psyllium and beet pulp provide particularly good results, helping to normalize water absorption and support healthy gut bacteria populations.
Elimination diets require strict adherence for 8-10 weeks without any treats, flavored medications, or unauthorized food items. During diet trials, dogs must consume only the prescribed food to accurately assess responses to specific ingredients.
Supportive Therapies
Dietary fiber supplements including psyllium, beet pulp, and fructooligosaccharides provide additional support for colon health. These supplements help normalize stool consistency while supporting beneficial bacteria populations in the intestinal tract.
Probiotics help restore beneficial bacteria populations disrupted by inflammation, stress, or antibiotic treatment. These supplements contain live bacteria strains that support gut health and may help prevent future episodes of colitis.
Prebiotics feed existing beneficial bacteria in the colon, helping them multiply and reestablish normal populations. These supplements work synergistically with probiotics to support overall digestive health and immune function.
Subcutaneous fluids may be necessary for dogs showing signs of dehydration, particularly in severe cases or when vomiting accompanies the diarrhea. This supportive care helps maintain hydration while other treatments address the underlying inflammation.
Managing Large Bowel Diarrhea
Managing large bowel diarrhea, a hallmark symptom of colitis in dogs, requires a thoughtful and multi-faceted approach to ensure your pet’s comfort and long-term health. The primary goal is to reduce the frequency and severity of diarrhea, address inflammation in the colon, and prevent complications such as dehydration and weight loss.
One of the most effective first steps is implementing a bland diet. Foods like boiled chicken and white rice are gentle on the digestive system and can help soothe the inflamed large bowel. Adding dietary fiber, such as psyllium husk or beet pulp, can further support gut health by regulating bowel movements and promoting the growth of beneficial bacteria in the colon. In some cases, your veterinarian may recommend a low-fiber diet instead, depending on your dog’s specific symptoms and response to treatment.
Medication often plays a key role in managing large bowel diarrhea. Anti inflammatory drugs can help reduce irritation and swelling in the colon, while targeted antibiotics may be necessary if a bacterial infection is present. Probiotics are also commonly used to restore the balance of beneficial bacteria, especially after antibiotic treatment or during periods of stress.
Stress management is another crucial aspect of treatment, as anxiety and environmental changes can trigger or worsen symptoms of colitis. Creating a calm, predictable environment, minimizing disruptions to your dog’s routine, and using stress-reducing aids like pheromone diffusers can all help to keep symptoms under control.
Regular veterinary check-ups are essential for monitoring your dog’s progress and adjusting the treatment plan as needed. Your veterinarian may recommend periodic blood tests and fecal exams to track your dog’s response to therapy and catch any early signs of complications. By working closely with your veterinarian and following a comprehensive plan that includes dietary changes, medication, and stress management, you can help your dog recover from large bowel diarrhea and maintain a healthy, happy life.


Recovery and Management
Most cases of acute colitis resolve within 24-48 hours to 3-5 days with appropriate treatment. Dogs typically show improvement in stool consistency and frequency within the first day or two of starting treatment, with complete resolution following shortly after.
Chronic colitis requires ongoing management but can be controlled effectively in most cases. While some chronic cases may not be completely curable, symptoms can be well-managed with appropriate diet and medication protocols. Long-term success depends on identifying and avoiding known triggers.
Regular monitoring helps track progress and adjust treatments as needed. Veterinarians typically schedule follow-up visits to assess response to treatment and modify protocols based on individual dog responses. Some dogs may need periodic medication adjustments or dietary modifications.
The prognosis for most dogs with colitis remains excellent, particularly for acute cases. Even dogs with chronic inflammatory bowel disease can live normal, comfortable lives with proper management and owner compliance with treatment recommendations.
Prevention Strategies
Avoiding sudden dietary changes represents one of the most effective prevention strategies. Gradual transitions over 5-7 days when changing foods help prevent digestive upset. Maintaining consistent, high-quality dog food reduces the risk of dietary-induced colitis episodes.
Minimizing stress through environmental management helps prevent stress colitis episodes. Maintaining routine schedules, providing safe spaces during stressful events, and using calming supplements during known triggers can significantly reduce colitis risk.
Regular parasite prevention and deworming as recommended by veterinarians helps prevent parasitic causes of colitis. Annual fecal examinations allow early detection and treatment of intestinal parasites before they cause significant symptoms.
Training dogs not to scavenge during walks and securing garbage prevents dietary indiscretions that commonly trigger acute colitis. Supervision during outdoor time and providing appropriate mental stimulation can reduce the likelihood of inappropriate eating behaviors.
When to Seek Emergency Care
Persistent diarrhea lasting more than 24-48 hours without improvement warrants immediate veterinary attention. While mild cases may resolve quickly, prolonged symptoms suggest more serious underlying conditions requiring professional treatment.
Signs of dehydration including dry gums, skin tenting, lethargy, and decreased urination indicate the need for emergency care. Dehydration can develop rapidly, particularly in puppies or elderly dogs, and requires prompt fluid therapy.
Severe abdominal pain, continuous vomiting, or complete loss of appetite suggest complications requiring immediate evaluation. These symptoms may indicate more serious conditions than simple colitis and need urgent medical attention.
Puppies, elderly dogs, or those with other medical conditions need immediate attention when colitis symptoms appear. These vulnerable populations can deteriorate rapidly and benefit from early intervention and supportive care.
Cost Considerations
Basic treatment costs include examination fees, fecal analysis, medications, and dietary changes. Initial veterinary visits for acute colitis typically range from moderate to higher expenses depending on geographic location and required testing.
Advanced diagnostics like ultrasound, colonoscopy, and specialized testing significantly increase expenses. These procedures become necessary for chronic cases or when initial treatments fail to provide adequate improvement.
Chronic cases require ongoing prescription diets and regular monitoring visits, creating long-term financial commitments. However, successful management often reduces overall costs compared to repeated acute episodes or emergency treatments.
Early intervention often reduces overall treatment costs compared to delayed care. Prompt treatment of acute colitis prevents progression to chronic conditions requiring more extensive and expensive management protocols.
FAQ
How long does it take for colitis to resolve in dogs?
Acute stress-related colitis typically resolves within 3-5 days with appropriate treatment including dietary changes and medications like metronidazole. Most dogs show significant improvement within 24-48 hours of starting treatment, with complete resolution following shortly after. Chronic colitis may take weeks to months to stabilize and often requires ongoing management with prescription diets and regular veterinary monitoring. Some dogs with inflammatory bowel disease need lifelong treatment but can live normal, comfortable lives with proper management.
Can I treat my dog’s colitis at home without veterinary care?
While mild cases may improve with bland diets and fasting, veterinary evaluation is essential to rule out serious underlying causes like parasites or infections. Home treatment should never include human medications, which can be toxic to dogs and worsen colitis symptoms. If symptoms persist beyond 24 hours or the dog shows signs of dehydration, immediate veterinary care is necessary to prevent complications. Professional diagnosis helps ensure appropriate treatment and prevents progression to chronic conditions.
What foods should I avoid feeding a dog with colitis?
Avoid high-fat foods, dairy products, spicy human foods, and any treats or table scraps that could irritate the inflamed colon. Skip foods with artificial additives, preservatives, and fillers that may trigger inflammatory responses in sensitive dogs. During elimination diet trials, strictly avoid all treats, flavored medications, and any food items not approved by your veterinarian. Sudden dietary changes should also be avoided, as gradual transitions help prevent digestive upset in dogs recovering from colitis.
Is colitis in dogs contagious to other pets or humans?
Colitis itself is not contagious, but some underlying causes like bacterial infections (Salmonella, E. coli) or parasites (Giardia) can spread between animals and potentially to humans. Practice good hygiene when handling affected dogs, including washing hands after cleanup and properly disposing of fecal matter. Have all household pets examined if one develops colitis to rule out infectious causes that could affect other animals. Most cases of stress-related or dietary-induced colitis pose no transmission risk to other pets or family members.
Can stress alone cause colitis in dogs, and how can I prevent it?
Yes, stress is one of the most common triggers for acute colitis in dogs, often called stress colitis by veterinarians. Common stressors include boarding, moving, travel, new pets, schedule changes, and environmental disruptions that affect your dog’s routine. Prevent stress-induced colitis by maintaining consistent routines, gradual introductions to changes, and using calming supplements or medications during known stressful events. Creating safe spaces and providing mental stimulation can also help dogs cope with unavoidable stressors more effectively.
FAQ
How long does it take for colitis to resolve in dogs?
Acute stress-related colitis typically resolves within 3-5 days with appropriate treatment including dietary changes and medications like metronidazole. Most dogs show significant improvement within 24-48 hours of starting treatment, with complete resolution following shortly after. Chronic colitis may take weeks to months to stabilize and often requires ongoing management with prescription diets and regular veterinary monitoring. Some dogs with inflammatory bowel disease need lifelong treatment but can live normal, comfortable lives with proper management.
Can I treat my dog’s colitis at home without veterinary care?
While mild cases may improve with bland diets and fasting, veterinary evaluation is essential to rule out serious underlying causes like parasites or infections. Home treatment should never include human medications, which can be toxic to dogs and worsen colitis symptoms. If symptoms persist beyond 24 hours or the dog shows signs of dehydration, immediate veterinary care is necessary to prevent complications. Professional diagnosis helps ensure appropriate treatment and prevents progression to chronic conditions.
What foods should I avoid feeding a dog with colitis?
Avoid high-fat foods, dairy products, spicy human foods, and any treats or table scraps that could irritate the inflamed colon. Skip foods with artificial additives, preservatives, and fillers that may trigger inflammatory responses in sensitive dogs. During elimination diet trials, strictly avoid all treats, flavored medications, and any food items not approved by your veterinarian. Sudden dietary changes should also be avoided, as gradual transitions help prevent digestive upset in dogs recovering from colitis.
Is colitis in dogs contagious to other pets or humans?
Colitis itself is not contagious, but some underlying causes like bacterial infections (Salmonella, E. coli) or parasites (Giardia) can spread between animals and potentially to humans. Practice good hygiene when handling affected dogs, including washing hands after cleanup and properly disposing of fecal matter. Have all household pets examined if one develops colitis to rule out infectious causes that could affect other animals. Most cases of stress-related or dietary-induced colitis pose no transmission risk to other pets or family members.
Can stress alone cause colitis in dogs, and how can I prevent it?
Yes, stress is one of the most common triggers for acute colitis in dogs, often called stress colitis by veterinarians. Common stressors include boarding, moving, travel, new pets, schedule changes, and environmental disruptions that affect your dog’s routine. Prevent stress-induced colitis by maintaining consistent routines, gradual introductions to changes, and using calming supplements or medications during known stressful events. Creating safe spaces and providing mental stimulation can also help dogs cope with unavoidable stressors more effectively.
Conclusion
Chronic colitis and other forms of colitis in dogs can be challenging, but with the right approach, most dogs can enjoy a good quality of life. Whether your dog’s colitis is triggered by dietary indiscretions, stress, or underlying bacterial infections, early recognition and prompt treatment are key to successful management. Working closely with your veterinarian to identify the underlying cause and develop a tailored treatment plan—including dietary changes, medication, and stress reduction—can make a significant difference in your dog’s recovery and long-term well-being.
Understanding the symptoms of colitis and taking action at the first sign of trouble can help prevent chronic issues and complications. If you suspect your dog has colitis, don’t hesitate to seek veterinary advice. With a combination of a balanced diet, regular check-ups, and a healthy lifestyle, you can help prevent future flare-ups and support your dog’s digestive health for years to come. Remember, most dogs with colitis—whether acute or chronic—can lead happy, active lives with the right care and attention.






