Key Takeaways
- Canine IVDD is the most common spinal disease in dogs, causing pain, paralysis, and mobility issues when disc material compresses the spinal cord
- Chondrodystrophic breeds like Dachshunds, Corgis, and French Bulldogs are at highest risk due to genetic predisposition on chromosome 12
- Early diagnosis and treatment are crucial—IVDD can significantly impact a dog's ability to move and perform normal activities, and recovery depends on the severity and location of the disc herniation. Dogs maintaining deep pain sensation have 90% surgical success rates for recovery
- Treatment ranges from conservative management with strict crate rest to emergency surgical decompression depending on severity
- Many dogs can return to normal function with proper treatment, though some may require mobility aids and ongoing care
Canine IVDD is the most common spinal disease in dogs, causing pain, paralysis, and mobility issues when disc material compresses the spinal cord
Chondrodystrophic breeds like Dachshunds, Corgis, and French Bulldogs are at highest risk due to genetic predisposition on chromosome 12
Early diagnosis and treatment are crucial—IVDD can significantly impact a dog's ability to move and perform normal activities, and recovery depends on the severity and location of the disc herniation. Dogs maintaining deep pain sensation have 90% surgical success rates for recovery
Treatment ranges from conservative management with strict crate rest to emergency surgical decompression depending on severity
Many dogs can return to normal function with proper treatment, though some may require mobility aids and ongoing care
When your dog suddenly yelps in pain, shows reluctance to move, or begins dragging their hind legs, intervertebral disc disease ivdd could be the underlying cause. This debilitating condition affects thousands of dogs annually, particularly certain breeds genetically predisposed to spinal problems. Understanding canine IVDD empowers pet owners to recognize early warning signs, seek appropriate treatment, and provide the best possible care for their affected companions.
Intervertebral disc disease represents one of the most common neurological conditions in veterinary medicine, with some breeds facing up to a 25% lifetime risk. While the diagnosis can feel overwhelming, advances in diagnostic imaging, surgical techniques, and rehabilitation protocols offer hope for dogs at every stage of the disease. From mild pain management to complex spinal surgery, treatment options continue expanding to help dogs maintain active, comfortable lives.
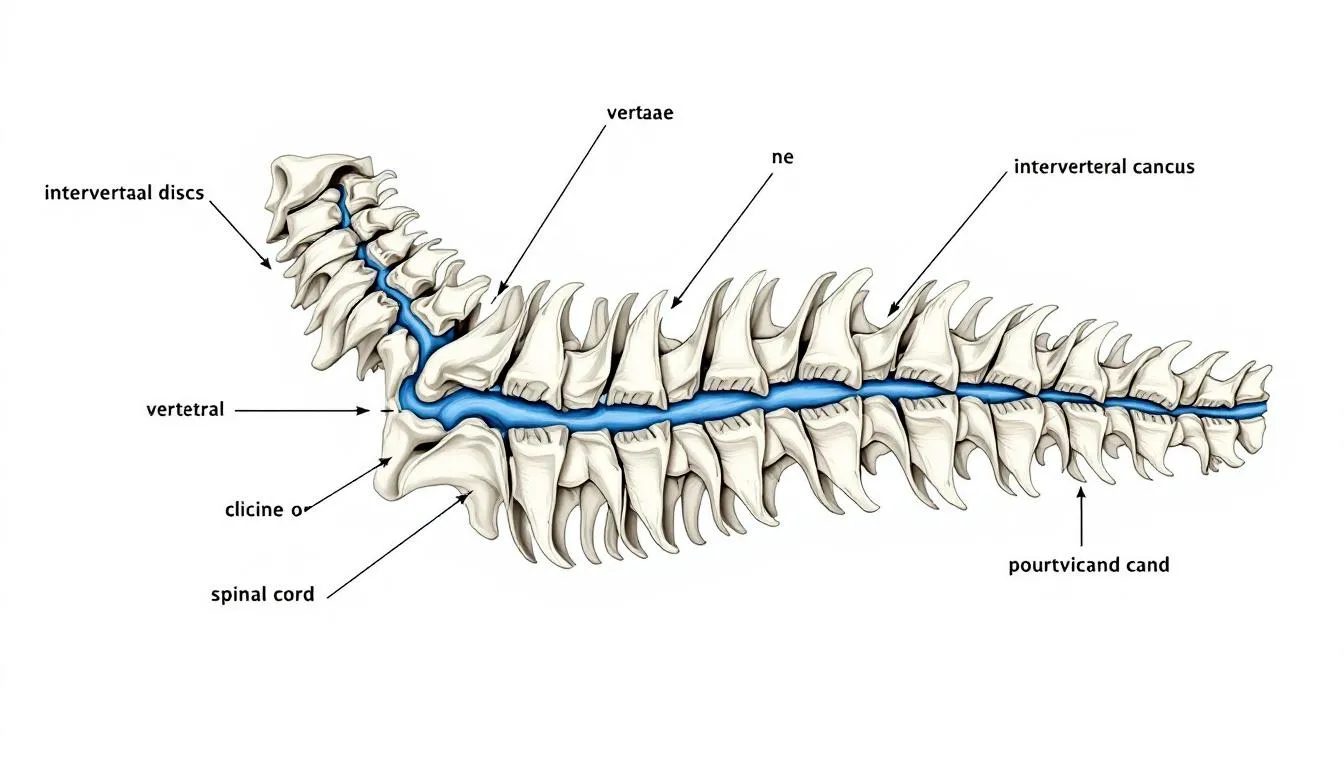
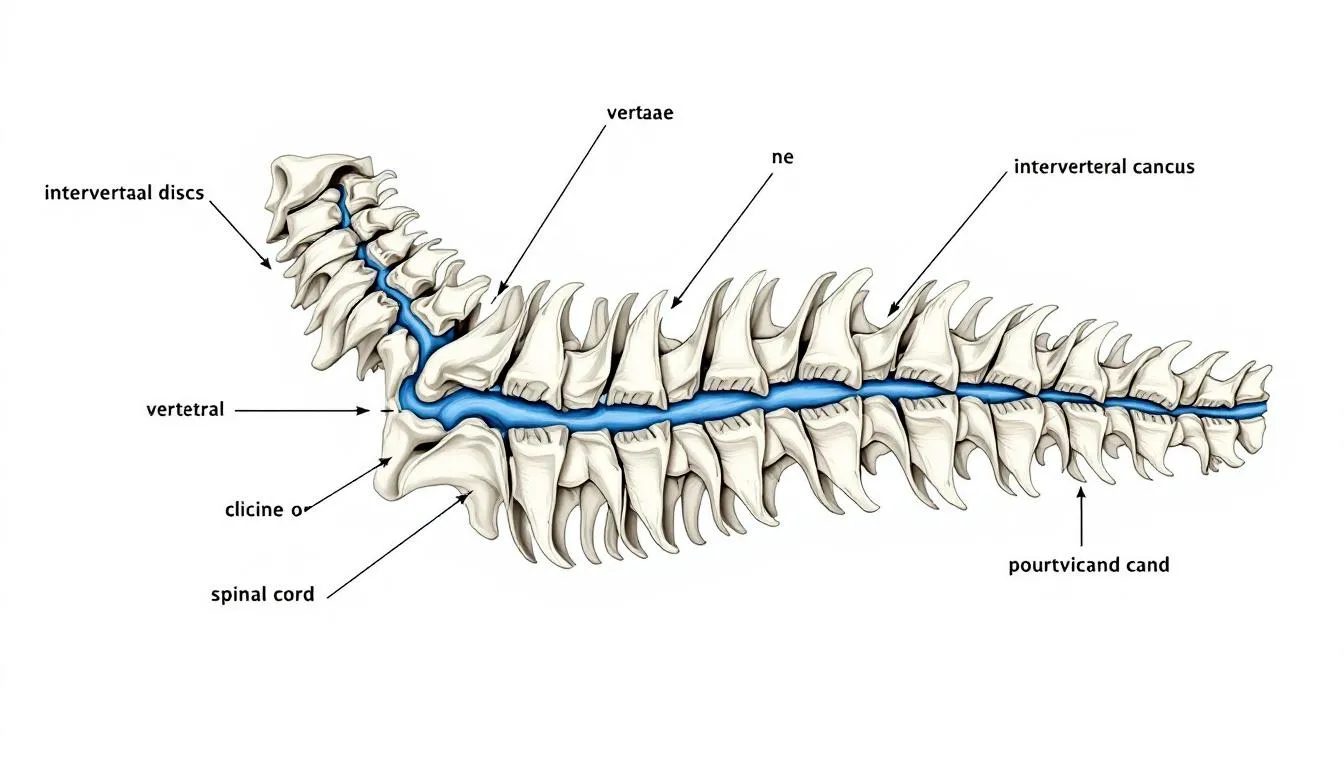
Understanding Canine IVDD: Definition and Anatomy
Intervertebral disc disease (IVDD), also known as intervertebral disk disease, occurs when the shock-absorbing cushions between vertebrae lose their structural integrity, leading to compression of the spinal cord or spinal nerves. These intervertebral discs serve as crucial components of the vertebral column (also referred to as the spinal column), providing flexibility while protecting the delicate nervous tissue within the spinal canal.
Each intervertebral disc consists of two primary structures: the tough outer layer called the annulus fibrosus and the gel-like inner core known as the nucleus pulposus. The discs are situated between the vertebral bodies, which are the bony structures of the spine. In healthy dogs, this design allows the spine to bend, twist, and absorb impact during normal activities. The hydrated nucleus pulposus extrusion occurs when degenerative changes weaken the outer layer, allowing the inner material to protrude into the vertebral canal. The lumbar vertebrae are a common site for disc herniation in dogs.
The process of disc degeneration typically begins with changes to the biochemical composition of the disc material. As dogs age or due to genetic factors, the nucleus pulposus loses its water content and becomes more fibrous. This transformation makes the disc less effective at absorbing shock and more prone to herniation (sometimes called a 'slipped disc') under normal mechanical stress.
When herniated disc material enters the spinal canal, it creates pressure on the dog’s spinal cord and surrounding spinal nerves. This spinal cord compression disrupts normal nerve transmission, leading to the characteristic symptoms of pain, weakness, and paralysis associated with disc disease in dogs. Disc extrusions refer to the extrusion of disc material causing spinal cord compression. The severity of symptoms depends on the amount of disc material impinges on neural structures and the speed at which compression develops.
Types of IVDD in Dogs
Veterinary medicine recognizes several distinct types of intervertebral disc degeneration, each with unique characteristics affecting diagnosis and treatment approaches. The traditional Hansen classification system provides the foundation for understanding these variations, though newer categories continue emerging through advanced imaging research.
Hansen Type I represents the most common form of acute spinal cord injury in susceptible breeds. This type ii disc disease involves sudden rupture of the annulus fibrosus, allowing calcified disc material to explosively enter the spinal canal. Compression of the spinal cord or nerves from herniated disc material can lead to reduced nerve function, resulting in neurological deficits such as weakness, loss of coordination, or even paralysis. Most disc ruptures of this type occur in chondrodystrophic breeds between two and seven years of age, often triggered by minor activities like jumping or playing.
Hansen Type II follows a much slower degenerative process, typically affecting large breed dogs between five and twelve years of age. Unlike the sudden extrusion seen in Type I, this condition involves gradual bulging of the disc into the vertebral canal. The slower degenerative process allows the spinal cord more time to adapt, often resulting in less severe clinical signs initially.
Hansen Type III, sometimes called acute non-compressive nucleus pulposus extrusion, presents a unique scenario where disc material explodes into the spinal canal but may not cause persistent compression. Dogs with this condition often show sudden onset of severe pain followed by rapid improvement, sometimes without surgical intervention.
Recent advances in magnetic resonance imaging have identified additional categories including hydrated nucleus pulposus extrusion and acute non-compressive nucleus pulposus extrusion. These classifications help veterinarians better understand the underlying pathology and select appropriate treatment strategies.
The severity of IVDD can range from mild pain to severe paralysis. In cases of moderate IVDD injury, dogs often benefit from strict activity restriction and medical management, with a generally favorable prognosis if treated promptly.
Breed-specific predispositions play a crucial role in determining which type of disc disease develops. Cervical ivdd occurs more frequently in small breeds, while thoracolumbar disc extrusion predominates in Dachshunds and similar breeds. Large breed dogs typically experience the chronic, progressive changes associated with Type II disease.


Clinical Signs and Symptoms
The clinical presentation of intervertebral disc herniation varies dramatically depending on the location, severity, and speed of onset. Early recognition of symptoms enables prompt intervention, which significantly improves treatment outcomes and prevents permanent neurological damage.
Initial signs often begin with subtle changes in behavior and mobility. Dogs may exhibit spinal pain through reluctance to jump onto furniture, difficulty navigating stairs, or abnormal posturing such as a hunched back. Many owners notice their pet becomes less active, shows decreased appetite, or displays unusual sensitivity when touched along the spine.
As the condition progresses, more obvious neurological deficits emerge. Hind limbs may show weakness, causing dogs to stumble or drag their rear legs. Some dogs develop an abnormal gait, walking with their hind legs spread wider than normal or showing obvious coordination problems. Cervical spine involvement typically produces front leg weakness and neck pain.
Advanced cases present with complete paralysis and loss of voluntary movement in affected limbs. The most critical assessment involves testing for deep pain sensation, which indicates the integrity of the deepest nerve pathways. Dogs that are deep pain negative face the most guarded prognosis and require emergency surgical intervention for any chance of recovery.
Bladder and bowel control often become compromised as the disease progresses. Early stages may show only occasional accidents, while severe cases result in complete loss of voluntary urination and defecation. In these cases, the patient's bladder may require manual expression to prevent dangerous over-distension and secondary complications.
Emergency warning signs include sudden onset of paralysis, complete loss of pain perception, or rapid deterioration of neurological function. These situations require immediate veterinary attention, as delays in treatment significantly reduce the chances of functional recovery.
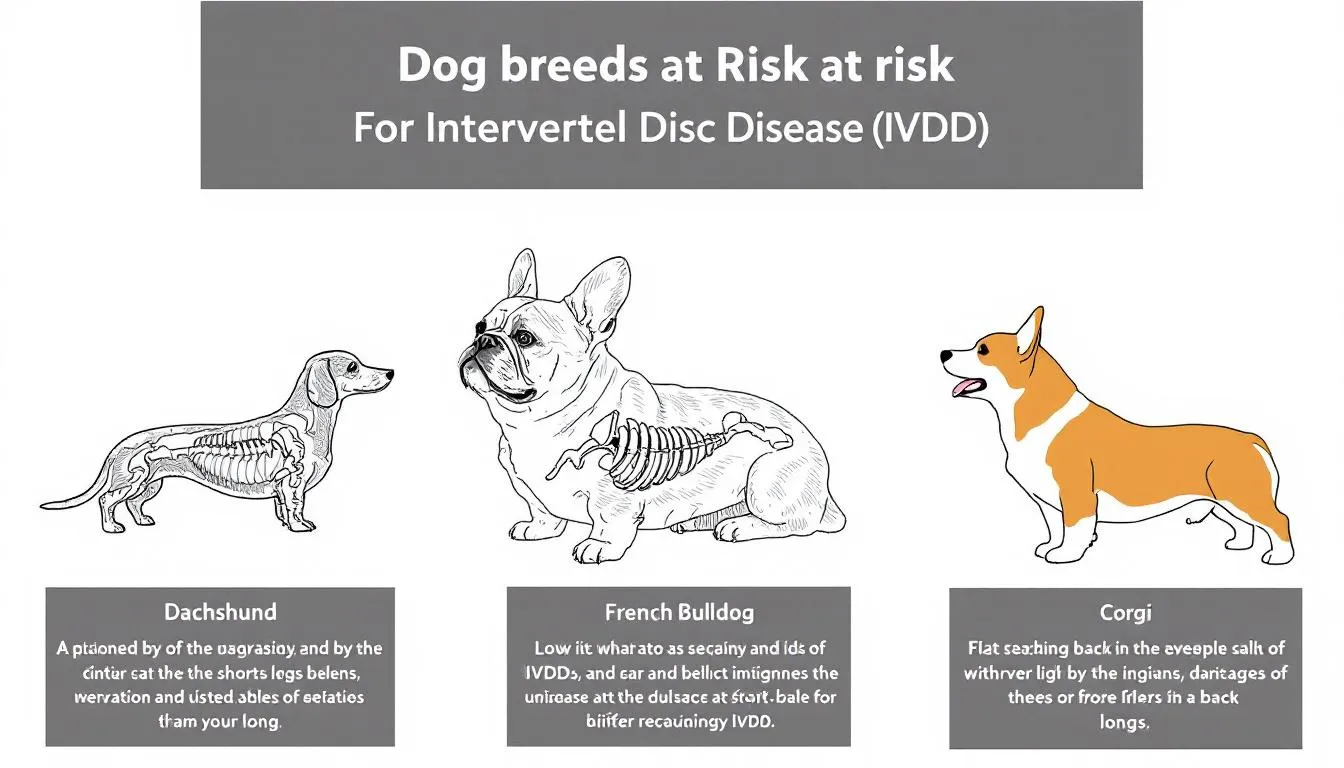
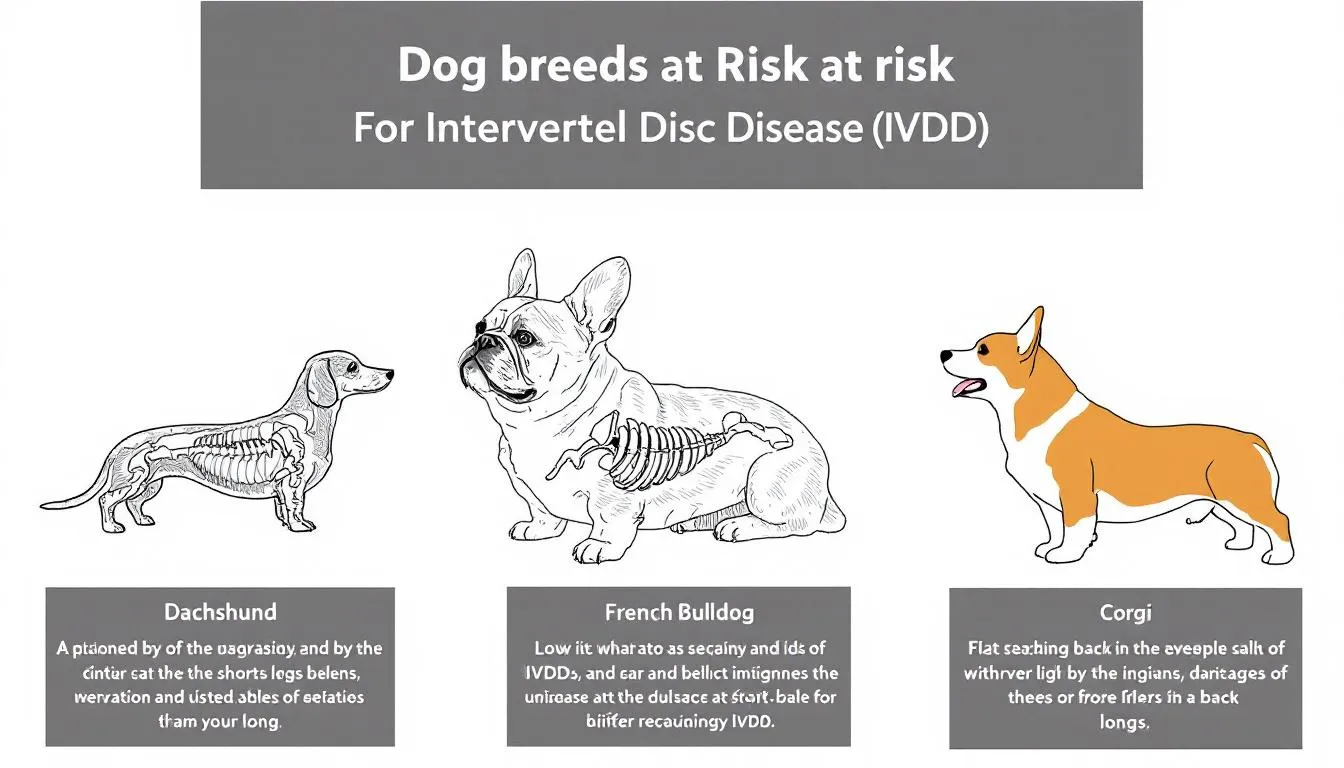
Breeds at Risk and Genetic Factors
Genetic predisposition plays the dominant role in determining which dogs develop intervertebral disc disease, with certain breeds showing dramatically elevated risk compared to mixed-breed dogs. Understanding these genetic factors helps owners of susceptible breeds implement preventive strategies and maintain heightened awareness for early symptoms.
Chondrodystrophic breeds represent the highest-risk category, with their characteristic long bodies and short legs creating biomechanical stress on the spine. Dachshunds face the greatest risk, with studies showing up to 25% of the breed developing clinically significant disc disease during their lifetime. French Bulldogs, Welsh Corgis, Basset Hounds, and Beagles also show markedly increased susceptibility.
Recent genetic research has identified the FGF4 retrogene on chromosome 12 as a primary factor in disc degeneration risk. This genetic variant affects cartilage development and predisposes affected breeds to premature disc aging. In susceptible breeds, significant disc degeneration may begin as early as three years of age, compared to much later onset in non-predisposed dogs.
Large breed dogs face different risk patterns, typically developing type ii disc disease later in life through mechanical wear and aging processes. German Shepherds, Labrador Retrievers, and Rottweilers show increased susceptibility compared to other large breeds, though their risk remains lower than chondrodystrophic breeds.
Age-related risk factors vary significantly by breed type. Predisposed breeds may show symptoms as young as two years old, with peak incidence occurring between three and six years. Large breed dogs typically develop symptoms between eight and twelve years of age, reflecting the different underlying disease processes.
Breeding programs increasingly incorporate genetic testing and radiographic screening to reduce IVDD prevalence. Responsible breeders avoid breeding dogs with family histories of severe disc disease and may utilize genetic tests when available. However, the complex inheritance patterns mean that even careful breeding cannot completely eliminate risk in susceptible breeds.
Diagnosis and Diagnostic Imaging
Accurate diagnosis of intervertebral disc disease requires a systematic approach combining clinical examination, neurological assessment, and advanced imaging techniques. Early and precise diagnosis enables appropriate treatment selection and improves long-term outcomes for affected dogs.
The diagnostic process begins with a thorough physical examination focusing on pain localization and neurological function assessment. Veterinarians evaluate the dog’s gait, posture, and response to spinal palpation to identify affected regions. Neurological testing includes assessment of reflexes, proprioception, and pain perception to determine the severity of spinal cord injury.
Basic blood work and urinalysis help evaluate the dog’s overall health status and identify any concurrent conditions that might complicate treatment. These tests become particularly important when considering surgical intervention or long-term medical management protocols.
Radiographs provide the initial imaging assessment, revealing calcified disc material, vertebral alignment, and disc space narrowing. While standard X-rays cannot directly visualize disc herniation, they help identify likely locations and rule out other spinal abnormalities such as fractures or tumors.
Advanced imaging represents the gold standard for definitive diagnosis and surgical planning. Magnetic resonance imaging provides unparalleled visualization of soft tissue structures, allowing precise identification of extruded disc material and assessment of spinal cord compression. MRI enables veterinarians to distinguish between different types of disc disease and evaluate the extent of spinal cord damage.
Computed tomography offers an alternative to MRI, particularly useful for visualizing calcified disc material and bony changes. CT scans require less time than MRI and may be more readily available in some regions, though they provide less detail about soft tissue structures and spinal cord condition.
Myelography, involving injection of contrast material around the spinal cord, may be utilized when MRI or CT scanning is unavailable. This technique can identify areas of spinal cord compression but carries higher risks and provides less detailed information than modern cross-sectional imaging methods.


Treatment Options
Conservative treatment approaches form the foundation of care for many dogs with mild to moderate intervertebral disc disease, offering effective pain relief and functional recovery without surgical intervention. Success with medical therapy depends on careful case selection, strict adherence to activity restrictions, and comprehensive supportive care.
Conservative Management
Strict crate rest represents the cornerstone of conservative management, typically prescribed for four to eight weeks depending on symptom severity. This enforced inactivity prevents further disc material from entering the spinal canal and allows natural healing processes to reduce inflammation around compressed neural structures. The confinement must be absolute, with dogs only leaving their crate for supervised bathroom breaks.
Pain management protocols typically combine multiple medication classes to address different aspects of discomfort. Gabapentin and pregabalin target neuropathic pain, while NSAIDs reduce inflammation and provide general analgesia. Muscle relaxants help address secondary muscle spasms that often accompany spinal injuries.
Bladder management becomes crucial for dogs with urinary retention or incontinence. Many dogs require assistance with bladder expression, performed through gentle manual pressure on the abdomen. Owners must learn proper techniques to prevent bladder over-distension while avoiding trauma to surrounding tissues.
Anti-inflammatory medications play a central role in reducing spinal cord edema and improving neurological function. Corticosteroids may provide rapid relief but require careful monitoring for side effects. Newer anti-inflammatory protocols focus on minimizing medication risks while maintaining therapeutic benefits.
Physical therapy begins during the acute phase with passive range-of-motion exercises and gradually progresses to active rehabilitation as symptoms improve. Early intervention helps prevent muscle atrophy and joint stiffness while promoting neurological recovery through controlled stimulation.
Success rates for conservative management vary by case severity, with mild cases showing 80-90% improvement rates. However, recurrence rates approach 30% in dogs with previous episodes, particularly when preventive measures are not consistently maintained.
Surgical Treatment
Surgical intervention provides the most effective treatment for severe cases of spinal cord compression, offering the best chance for neurological recovery when performed promptly. The decision for spinal surgery depends on symptom severity, rate of progression, and response to initial medical management.
Emergency surgery becomes indicated when dogs lose deep pain sensation, develop complete paralysis, or show rapid neurological deterioration. The window for effective intervention is critical, with best outcomes achieved when surgical decompression occurs within 24 hours of losing deep pain perception.
Hemilaminectomy represents the most commonly performed procedure for thoracolumbar disc extrusion. This technique involves removing a portion of the vertebral bone overlying the spinal cord, allowing access to remove extruded disc material and decompress neural structures. The procedure preserves spinal stability while providing adequate visualization of the affected area.
Ventral slot decompression addresses cervical spine problems through an approach from the underside of the neck. This technique allows direct access to disc material compressing the spinal cord from below while maintaining the structural integrity of the cervical vertebrae.
Dorsal laminectomy procedures remove larger portions of vertebral bone to access the spinal canal from above. This approach may be necessary for extensive compressions or when multiple disc spaces require attention during a single surgical session.
Prophylactic fenestration involves removing disc material from adjacent, non-herniated discs to prevent future episodes. This technique may be performed simultaneously with decompressive surgery or as a standalone procedure in high-risk patients with early degenerative changes.
Surgical success rates vary dramatically based on preoperative neurological status. Dogs maintaining deep pain sensation achieve functional recovery in 80-90% of cases, while those without pain perception recover in approximately 50% of cases. The speed of surgical intervention significantly influences these outcomes.
Surgery Costs and Financial Considerations
The financial aspects of IVDD treatment, particularly surgical intervention, represent a significant consideration for many pet owners facing this diagnosis. Understanding the full scope of expenses enables families to make informed decisions and plan appropriately for their dog’s care.
Typical surgical costs range from $2,000 to $5,000 for standard decompressive procedures, with complex cases or emergency surgeries potentially exceeding these estimates. Geographic location, specialist availability, and hospital facilities all influence final costs. Urban areas and specialty centers typically charge higher fees than general practice clinics.
Pre-operative expenses include diagnostic imaging, blood work, anesthesia evaluation, and specialist consultations. Advanced imaging alone may cost $1,000 to $2,500, depending on the specific techniques required and regional pricing variations. These diagnostic costs remain necessary even if owners ultimately choose conservative treatment.
Post-operative care expenses continue well beyond the initial surgery, including hospitalization, pain medications, follow-up examinations, and potential complications management. Hospital stays typically last 2-5 days for routine cases, with extended stays required for dogs experiencing delayed recovery or complications.
Rehabilitation and physical therapy programs add additional costs but significantly improve recovery outcomes. Professional rehabilitation may cost $100-200 per session, with treatment courses extending 4-12 weeks depending on individual progress. Home exercise programs can reduce these costs while maintaining therapeutic benefits.
Pet insurance coverage varies significantly among providers and policy types, with many plans excluding pre-existing conditions. Owners of high-risk breeds should consider insurance early in their dog’s life, before any symptoms develop. Some policies specifically cover alternative treatments like acupuncture and hydrotherapy.
Financial assistance programs exist through veterinary schools, charitable organizations, and some specialty practices. Care Credit and similar medical financing options provide payment plans for qualified applicants. Some practices offer package pricing for combined diagnostic and treatment services.


Recovery and Prognosis
The recovery process following IVDD treatment varies dramatically among individual dogs, influenced by factors including initial severity, treatment method, patient age, and underlying health status. Understanding realistic expectations helps owners provide appropriate support while maintaining hope for optimal outcomes.
Hospital discharge typically occurs when dogs regain independent urination or owners demonstrate competency with bladder expression techniques. Most surgical patients remain hospitalized 2-5 days, while dogs receiving conservative treatment may go home immediately with strict activity restrictions.
Recovery timelines extend from weeks to months, with gradual improvement being the norm rather than dramatic sudden changes. Early improvements often include increased alertness, improved appetite, and reduced pain levels. Neurological recovery typically follows a predictable pattern, beginning with deep sensation return, followed by voluntary movement, and finally coordinated walking.
Dogs maintaining deep pain sensation before treatment show the most favorable prognosis, with 90% achieving functional recovery within 2-6 months. Those losing pain perception face more guarded outcomes, though 50% still regain meaningful function with appropriate treatment and rehabilitation.
Physical therapy plays a crucial role in optimizing recovery outcomes, beginning with passive range-of-motion exercises during hospitalization and progressing to active rehabilitation as neurological function returns. Hydrotherapy, therapeutic massage, and controlled exercise programs all contribute to improved strength and coordination.
Functional recovery varies from complete return to normal activity to partial improvement requiring ongoing support. Many dogs achieve sufficient recovery to enjoy walks, play, and normal household activities, even if they don’t return to pre-injury athletic performance levels.
Long-term prognosis includes consideration of recurrence risk, which affects approximately 30% of dogs with previous IVDD episodes. Preventive measures, weight management, and activity modifications help reduce this risk while maintaining quality of life.
Post-Treatment Care and Rehabilitation
Successful recovery from IVDD requires comprehensive post-treatment care extending well beyond initial hospitalization or acute treatment phases. Proper rehabilitation protocols, environmental modifications, and ongoing monitoring significantly influence long-term outcomes and quality of life.
Activity restriction protocols must be strictly maintained during initial healing phases, typically lasting 4-8 weeks following surgery or during conservative treatment. Dogs require complete confinement except for supervised bathroom breaks, with gradual activity increases only as directed by veterinary professionals.
Physical rehabilitation begins with passive exercises during acute phases and progresses to active programs as neurological function returns. Range-of-motion exercises prevent joint stiffness and muscle contracture, while sensory stimulation promotes neural pathway regeneration. Professional rehabilitation therapists design individualized programs targeting specific deficits.
Bladder and bowel management requires ongoing attention in many cases, particularly during early recovery phases. Owners must learn proper expression techniques, maintain regular schedules, and monitor for complications such as urinary tract infections or skin irritation from incontinence.
Home environment modifications enhance safety and accessibility for dogs with mobility limitations. Non-slip surfaces, ramps instead of stairs, and elevated food and water bowls reduce strain on healing spines. Baby gates can restrict access to dangerous areas like stairs or furniture.
Regular follow-up appointments allow veterinarians to monitor healing progress, adjust medications, and identify potential complications early. Neurological examinations track recovery patterns while imaging studies may be repeated if progress stalls or symptoms worsen.
Pain management evolves throughout the recovery process, with medications adjusted based on activity levels and healing progress. Long-term pain control may require multimodal approaches combining pharmaceuticals with physical therapy and environmental modifications.
Mobility Aids and Adaptive Equipment
When dogs experience permanent mobility impairment following IVDD, various assistive devices and adaptive equipment can restore independence and maintain quality of life. Modern mobility aids enable many paralyzed dogs to remain active, social, and engaged with their families.
Custom-fitted wheelchairs provide the most comprehensive mobility solution for dogs with hind limb paralysis. These devices support the rear body while allowing normal front leg function for steering and propulsion. Proper fitting ensures comfort and prevents pressure sores or additional injuries.
Harnesses and slings offer temporary or partial support for dogs with weakness rather than complete paralysis. These devices assist walking while maintaining some independent movement, making them ideal for dogs in recovery phases or with mild ongoing deficits.
Ramps and non-slip surfaces throughout the home environment prevent falls and reduce strain on healing spines. Rubber matting, carpet runners, and textured surfaces provide traction on smooth floors, while ramps eliminate the need for jumping or climbing stairs.
Specialized bladder expression equipment and positioning aids help owners maintain proper hygiene and prevent complications. Waterproof bedding, absorbent pads, and protective clothing reduce cleanup while maintaining skin health.
Quality of life assessments help families determine when mobility aids enhance rather than burden their dog’s daily experience. Many dogs adapt quickly to wheelchairs and other devices, resuming active, happy lives with appropriate support.
Professional fitting and training ensure optimal outcomes with mobility equipment. Veterinary rehabilitation specialists and certified equipment providers offer guidance on device selection, proper fitting, and training protocols for both dogs and owners.
Prevention and Risk Reduction
Preventing IVDD or reducing its severity requires a multifaceted approach combining genetic awareness, lifestyle modifications, and environmental management. While genetic predisposition cannot be changed, many risk factors remain modifiable through owner intervention.
Weight management represents the single most important preventive measure for all dogs, particularly those in high-risk breeds. Excess weight increases mechanical stress on intervertebral discs while promoting inflammatory processes that accelerate degeneration. Maintaining lean body condition reduces IVDD risk by up to 50% in susceptible breeds.
Exercise modification focuses on avoiding high-impact activities that stress the spine while maintaining appropriate fitness levels. Swimming provides excellent low-impact exercise, while controlled leash walks on flat surfaces minimize spinal stress. Avoiding jumping, stair climbing, and rough play reduces acute injury risk.
Environmental modifications within the home reduce daily spinal stress and injury risk. Ramps to furniture and cars, non-slip surfaces, and elevated food bowls minimize awkward positioning and sudden movements that can trigger disc herniation.
Early intervention programs for high-risk breeds include regular neurological examinations, weight monitoring, and owner education about warning signs. Some veterinarians recommend prophylactic imaging in asymptomatic dogs from susceptible breeds to identify early degenerative changes.
Genetic testing and responsible breeding practices help reduce IVDD prevalence in future generations. Breeders increasingly utilize available genetic tests and avoid breeding dogs with family histories of severe disc disease, though the complex inheritance patterns limit complete prevention.
Nutritional support may play a role in maintaining disc health, with some evidence supporting omega-3 fatty acids and joint supplements. While not proven to prevent IVDD, these interventions pose minimal risk and may provide additional benefits for overall joint health.
Complications and Emergency Situations
IVDD treatment and recovery can be complicated by various secondary conditions and emergency situations requiring immediate intervention. Understanding these potential complications enables owners to recognize warning signs and seek appropriate care promptly.
Progressive myelomalacia represents the most devastating complication, involving ascending destruction of spinal cord tissue. This condition typically develops 2-7 days after initial injury and carries a grave prognosis. Warning signs include ascending paralysis, loss of function in previously normal limbs, and deteriorating neurological status despite treatment.
Urinary tract complications frequently develop in dogs with bladder dysfunction, including infections, bladder stones, and chronic retention. Regular monitoring, proper expression techniques, and prophylactic antibiotics help prevent these secondary problems that can significantly impact recovery and quality of life.
Pressure sores and skin breakdown present ongoing challenges for immobile dogs, particularly over bony prominences like hips and elbows. Prevention requires frequent position changes, appropriate bedding, and vigilant skin care. Once established, pressure sores heal slowly and may become infected.
Recurrent disc herniations at different spinal levels affect approximately 30% of dogs with previous episodes. New episodes may involve the same location or different disc spaces, requiring fresh diagnostic workup and treatment decisions. Prevention focuses on continued activity restrictions and weight management.
Emergency situations requiring immediate veterinary attention include sudden loss of previously returned function, signs of progressive myelomalacia, severe breathing difficulties in cervical cases, and inability to urinate for more than 12 hours. These complications can rapidly become life-threatening without prompt intervention.
Chronic pain management challenges arise when dogs develop persistent discomfort despite appropriate treatment. Multimodal pain control approaches, including pharmaceuticals, physical therapy, and alternative treatments like acupuncture, may be necessary for maintaining comfort and function.
FAQ
Can dogs with IVDD live normal lives after treatment?
Many dogs with IVDD can return to active, happy lives following successful treatment, though the definition of “normal” may vary. Dogs treated early in the disease process, particularly those maintaining deep pain sensation, have excellent chances of resuming most pre-injury activities. Some may require ongoing activity modifications, such as avoiding jumping or high-impact exercise, but can still enjoy walks, play, and social interactions. Dogs with permanent mobility impairments often adapt well to wheelchairs and other assistive devices, maintaining good quality of life with appropriate support.
How long does it take for a dog to recover from IVDD surgery?
Recovery timelines vary significantly based on pre-surgical neurological status and individual factors. Dogs with mild deficits may show improvement within days to weeks, while those with severe injuries may require 3-6 months for maximum recovery. Initial improvements often include return of sensation and voluntary movement, followed by gradual strengthening and coordination improvements. Physical therapy significantly influences recovery speed, with structured rehabilitation programs often reducing overall recovery time compared to rest alone.
What are the chances my dog will walk again after losing deep pain sensation?
Dogs that lose deep pain sensation face more guarded prognoses, with approximately 50% regaining functional walking ability following prompt surgical intervention. The timing of surgery becomes critical, with best outcomes achieved within 24 hours of losing pain perception. Even dogs that don’t recover walking ability may regain some neurological function and can often live comfortable lives with mobility aids. Each case is unique, and recovery potential depends on factors including the extent of spinal cord damage, surgical timing, and individual healing capacity.
How can I prevent my dog from developing IVDD if they’re a high-risk breed?
Prevention strategies focus on reducing modifiable risk factors while acknowledging that genetic predisposition cannot be changed. Maintaining optimal weight reduces spinal stress by up to 50% in susceptible breeds. Avoid high-impact activities like jumping on and off furniture, using stairs frequently, or engaging in rough play. Provide ramps for car access and elevated surfaces, use harnesses instead of collars, and maintain regular exercise through controlled, low-impact activities like swimming. Early recognition of symptoms enables prompt treatment, which significantly improves outcomes even when prevention isn’t completely possible.
Is it better to choose surgery or conservative treatment for my dog’s IVDD?
The choice between surgical and conservative treatment depends on several factors including neurological severity, rate of symptom progression, and individual circumstances. Dogs with mild symptoms and intact pain sensation often respond well to conservative management with strict rest and medical therapy. Surgery becomes necessary for dogs with severe neurological deficits, complete paralysis, or rapid deterioration. Those losing deep pain sensation require emergency surgery for any chance of recovery. Your veterinarian will assess your dog’s specific situation and discuss the pros and cons of each approach, considering factors like age, overall health, and family preferences alongside medical factors.
FAQ
Can dogs with IVDD live normal lives after treatment?
Many dogs with IVDD can return to active, happy lives following successful treatment, though the definition of “normal” may vary. Dogs treated early in the disease process, particularly those maintaining deep pain sensation, have excellent chances of resuming most pre-injury activities. Some may require ongoing activity modifications, such as avoiding jumping or high-impact exercise, but can still enjoy walks, play, and social interactions. Dogs with permanent mobility impairments often adapt well to wheelchairs and other assistive devices, maintaining good quality of life with appropriate support.
How long does it take for a dog to recover from IVDD surgery?
Recovery timelines vary significantly based on pre-surgical neurological status and individual factors. Dogs with mild deficits may show improvement within days to weeks, while those with severe injuries may require 3-6 months for maximum recovery. Initial improvements often include return of sensation and voluntary movement, followed by gradual strengthening and coordination improvements. Physical therapy significantly influences recovery speed, with structured rehabilitation programs often reducing overall recovery time compared to rest alone.
What are the chances my dog will walk again after losing deep pain sensation?
Dogs that lose deep pain sensation face more guarded prognoses, with approximately 50% regaining functional walking ability following prompt surgical intervention. The timing of surgery becomes critical, with best outcomes achieved within 24 hours of losing pain perception. Even dogs that don’t recover walking ability may regain some neurological function and can often live comfortable lives with mobility aids. Each case is unique, and recovery potential depends on factors including the extent of spinal cord damage, surgical timing, and individual healing capacity.
How can I prevent my dog from developing IVDD if they’re a high-risk breed?
Prevention strategies focus on reducing modifiable risk factors while acknowledging that genetic predisposition cannot be changed. Maintaining optimal weight reduces spinal stress by up to 50% in susceptible breeds. Avoid high-impact activities like jumping on and off furniture, using stairs frequently, or engaging in rough play. Provide ramps for car access and elevated surfaces, use harnesses instead of collars, and maintain regular exercise through controlled, low-impact activities like swimming. Early recognition of symptoms enables prompt treatment, which significantly improves outcomes even when prevention isn’t completely possible.
Is it better to choose surgery or conservative treatment for my dog’s IVDD?
The choice between surgical and conservative treatment depends on several factors including neurological severity, rate of symptom progression, and individual circumstances. Dogs with mild symptoms and intact pain sensation often respond well to conservative management with strict rest and medical therapy. Surgery becomes necessary for dogs with severe neurological deficits, complete paralysis, or rapid deterioration. Those losing deep pain sensation require emergency surgery for any chance of recovery. Your veterinarian will assess your dog’s specific situation and discuss the pros and cons of each approach, considering factors like age, overall health, and family preferences alongside medical factors.
Cervical IVDD: Special Considerations
Cervical Intervertebral Disc Disease (IVDD) refers to disc disease affecting the neck region, or cervical spine, of a dog. While less common than thoracolumbar IVDD, cervical IVDD can be particularly distressing due to the sensitive anatomy and the vital functions controlled by the cervical spinal cord. Dogs with cervical IVDD often present with severe pain, reluctance to move the head or neck, and sometimes neurological deficits such as weakness or unsteadiness in all four limbs. In some cases, even mild manipulation of the neck can trigger intense discomfort or muscle spasms.
Diagnosing cervical IVDD requires careful clinical evaluation and advanced diagnostic imaging. Magnetic resonance imaging (MRI) is especially valuable for visualizing the extent of spinal cord compression and pinpointing the affected intervertebral disc. Because the cervical spine is a complex and delicate area, accurate diagnosis is essential for planning effective treatment and minimizing the risk of further injury.
Treatment for cervical IVDD may begin with conservative management, including strict rest, pain relief, and physical therapy to reduce inflammation and support recovery. However, due to the risk of rapid deterioration and the potential for severe neurological impairment, surgical intervention is often recommended for dogs with significant spinal cord compression or persistent pain. Procedures such as ventral slot decompression are designed to remove the problematic disc material and relieve pressure on the spinal cord, offering the best chance for a full recovery.
Early recognition and prompt treatment are critical in cases of cervical IVDD. With timely intervention—whether through conservative management or surgery—many dogs can regain comfort and mobility, avoiding long-term complications and enjoying a good quality of life.
Disc Extrusion: What It Means and How It’s Treated
Disc extrusion, commonly referred to as a herniated disc, occurs when the soft, inner core of the intervertebral disc (the nucleus pulposus) pushes through a tear in the tough outer layer (the annulus fibrosus). When this extruded disc material enters the spinal canal, it can compress the spinal cord or nearby nerves, leading to pain, weakness, or even paralysis depending on the severity and location of the extrusion.
Disc extrusion is often the result of underlying disc degeneration, but it can also be triggered by trauma or genetic predisposition. The sudden pressure from the extruded disc material can cause acute symptoms, such as yelping in pain, reluctance to move, or loss of coordination in the limbs. In severe cases, dogs may lose the ability to walk or control their bladder and bowel functions.
Treatment for disc extrusion depends on the degree of spinal cord compression and the dog’s neurological status. Mild cases may respond well to conservative management, including pain relievers, anti-inflammatory medications, and physical therapy to support healing and restore function. However, when extruded disc material causes significant spinal cord compression or rapid neurological decline, surgical intervention is often necessary. Spinal surgery, such as a hemilaminectomy or ventral slot decompression, is performed to remove the extruded disc material and relieve pressure on the spinal cord, giving the best chance for neurological recovery.
Prompt diagnosis and appropriate treatment are essential to prevent permanent spinal cord injury. With early intervention—whether through conservative management or surgical decompression—many dogs can recover mobility and return to a happy, active life.
Intervertebral Discs and Hydration: The Science of Disc Health
Intervertebral discs are remarkable, hydrated structures that act as shock absorbers between the vertebrae, allowing the spine to move flexibly while protecting the spinal cord. The health of these discs depends largely on their water content, which keeps them spongy and resilient. Well-hydrated intervertebral discs can effectively cushion the spine and distribute pressure during movement, reducing the risk of injury.
As dogs age, or due to genetic and lifestyle factors, the discs can lose hydration—a process known as disc degeneration. Dehydrated discs become less elastic and more prone to cracking or herniation, which can lead to intervertebral disc disease (IVDD). This degeneration is a key factor in the development of disc disease in dogs, especially in breeds predisposed to IVDD.
Maintaining disc hydration and overall spinal health involves several proactive steps. Keeping your dog at a healthy weight reduces unnecessary stress on the intervertebral discs. Regular, low-impact exercise helps maintain flexibility and muscle support for the spine. Avoiding activities that place excessive strain on the back, such as jumping from heights or rough play, can also help preserve disc integrity.
Advanced imaging techniques, such as magnetic resonance imaging (MRI), allow veterinarians to assess the hydration and condition of intervertebral discs. Early detection of disc degeneration through advanced imaging can guide preventive care and timely intervention, helping to manage or even prevent intervertebral disc disease ivdd.
By understanding the importance of disc hydration and taking steps to support spinal health, dog owners can help their pets avoid the pain and mobility issues associated with disc disease. Regular veterinary check-ups, a balanced lifestyle, and early attention to any signs of back pain are key to ensuring your dog enjoys a happy and active life.






