Key Takeaways
-
Canine ehrlichiosis is a serious tick-borne disease caused primarily by Ehrlichia canis bacteria transmitted through brown dog tick bites
-
The disease progresses through three distinct phases: acute (fever, lethargy), subclinical (hidden symptoms), and chronic (severe complications including bleeding disorders)
-
German Shepherds and Doberman Pinschers are genetically predisposed to developing severe forms of ehrlichiosis
-
Early diagnosis and treatment with doxycycline for at least 28 days typically results in excellent recovery outcomes
-
Year-round tick prevention using topical treatments, oral medications, or collars is the most effective way to protect dogs from infection
What is Canine Ehrlichiosis?
Canine ehrlichiosis represents a complex group of infectious diseases caused by bacteria belonging to the Ehrlichia genus. Several species of Ehrlichia can infect dogs and other animals, highlighting the diversity of pathogens responsible for ehrlichiosis. These microscopic organisms are classified as rickettsiae-obligate intracellular bacteria that can only survive and reproduce inside living host cells. The most clinically significant pathogen affecting dogs is Ehrlichia canis, which causes canine monocytic ehrlichiosis by specifically targeting white blood cells called monocytes.
The disease earned its historical moniker "tracker dog disease" and "tropical canine pancytopenia" during the Vietnam War, when many military working dogs developed severe illness characterized by dangerous drops in blood cell counts. This tragic period led to increased research and understanding of the condition, ultimately benefiting countless dogs worldwide.
Ehrlichia canis (E canis) is the primary pathogen responsible for most cases of canine ehrlichiosis. It primarily infects white blood cells, specifically monocytes, where the bacteria multiply and spread throughout the body. This invasion triggers an immune system response that, while attempting to fight the infection, often contributes to many of the clinical symptoms observed in infected dogs. The worldwide distribution of this disease correlates directly with the presence of competent tick vectors, making geographic awareness crucial for both veterinarians and pet owners.
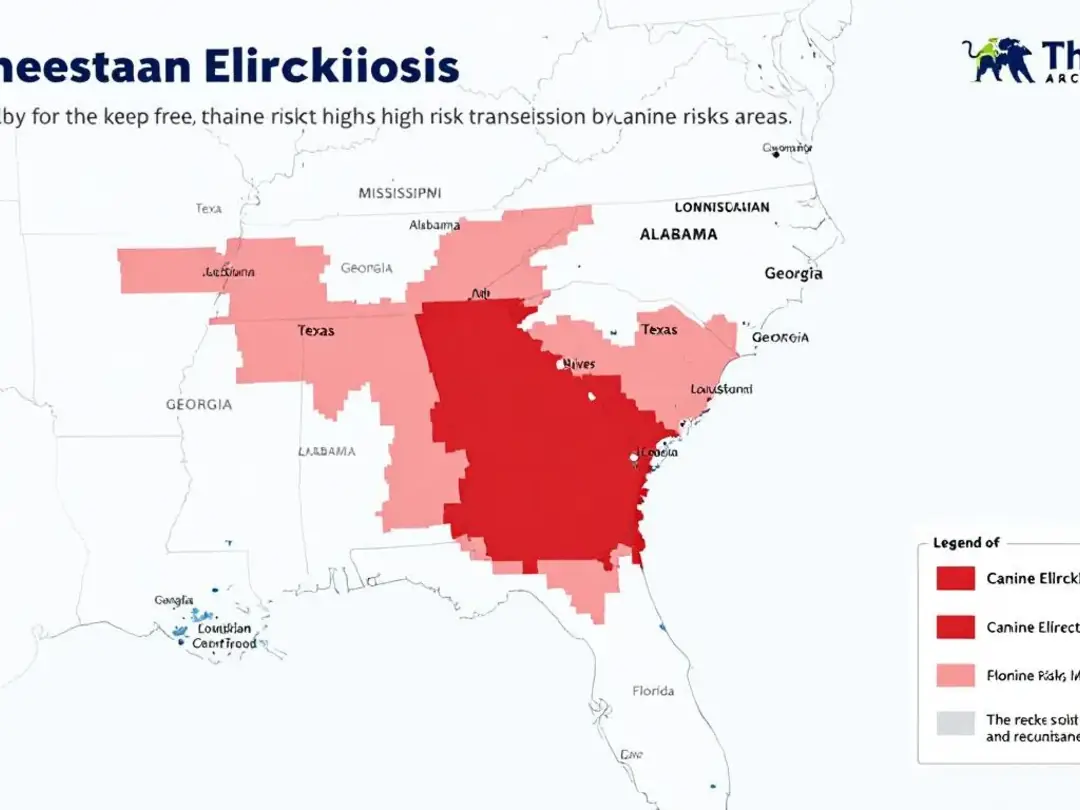
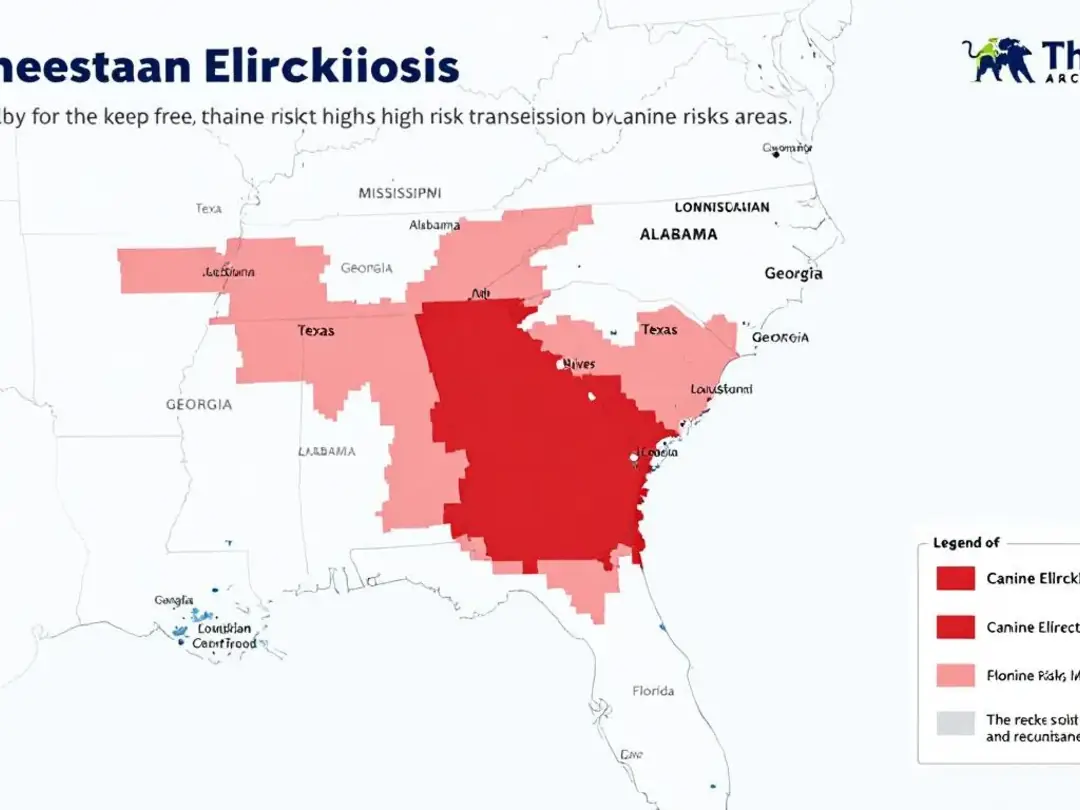
The southeastern and southwestern United States show the highest prevalence rates, with some endemic areas reporting seroprevalence rates exceeding 10-20% in local dog populations. This geographic clustering reflects both environmental factors favoring tick survival and the concentration of susceptible host animals. In canis infections, the progression from acute to chronic stages can lead to significant organ changes, further complicating clinical management.
How Dogs Become Infected
The brown dog tick, scientifically known as Rhipicephalus sanguineus, serves as the primary vector for Ehrlichia canis transmission. Unlike many other tick species that prefer wild animals and other infected animals as hosts, the brown dog tick shows a remarkable adaptability to domestic environments, making it particularly dangerous for pet dogs.
Transmission occurs when an infected tick feeds on a dog for several hours. The bacteria must migrate from the tick's salivary glands into the bloodstream, a process requiring 3-6 hours of continuous attachment. This timeline provides a critical window for prevention-daily tick checks and prompt removal can significantly reduce infection risk. There is no direct transmission risk from dogs to humans; transmission requires a tick vector.
Other tick species play roles in transmitting different Ehrlichia subspecies. The lone star tick (Amblyomma americanum) can transmit E. ewingii, which causes canine granulocytic ehrlichiosis, while the American dog tick and black-legged tick may carry additional species. Other infected animals can serve as reservoirs for the bacteria, contributing to the disease cycle. Understanding your local tick population helps assess specific risks for your region.
Risk factors for ehrlichia canis infection include outdoor activities in wooded or brushy areas, particularly during warmer months when ticks are most active. Dogs that hunt, hike, or spend significant time in rural environments face elevated exposure risks. Even urban dogs aren't immune-brown dog ticks can establish populations in homes, kennels, and yards.
A rare but documented transmission route involves blood transfusions from infected donor dogs. This highlights the importance of screening donor animals and represents why many veterinary blood banks maintain strict testing protocols.
Breed Predisposition and Risk Factors
Genetic factors significantly influence disease severity and progression in canine ehrlichiosis. German Shepherd Dogs demonstrate increased susceptibility to severe forms of the disease, with a higher likelihood of developing chronic ehrlichiosis that proves difficult to treat. This breed predisposition appears linked to immune system variations that affect how effectively dogs can clear the bacterial infection.
Doberman Pinschers share similar genetic vulnerabilities, often progressing to chronic phases characterized by severe bleeding disorders and bone marrow suppression. Siberian Huskies also show elevated risk for serious complications, including the development of aplastic anemia-a life-threatening condition where bone marrow fails to produce adequate blood cells.
Age-related factors influence infection patterns, with adult dogs more commonly affected than puppies. This may reflect increased outdoor exposure over time rather than inherent age-based susceptibility. However, very young and elderly dogs may experience more severe clinical signs due to immature or compromised immune systems.
Seasonal patterns align with tick activity cycles, showing peak transmission during warmer months when tick populations are most active. In southern climates with year-round tick activity, infections can occur throughout the year, necessitating continuous prevention measures.
Geographic risk zones encompass much of the southern United States, with Arkansas, Louisiana, Oklahoma, Tennessee, and Texas representing particular hotspots. Dogs traveling to or living in these endemic areas require heightened vigilance and robust tick prevention protocols.


Clinical Signs and Disease Progression
Understanding the three-phase progression of canine ehrlichiosis is crucial for early recognition and successful treatment. While some dogs recover after the acute phase, others may develop a chronic infection, which can lead to persistent symptoms and organ involvement such as splenomegaly, organ failure, and hematologic abnormalities. Each phase presents distinct clinical signs and diagnostic challenges that require veterinary attention, and the disease can manifest differently in each infected dog depending on the stage and severity of infection.
Acute Phase (1-3 weeks post-infection)
The acute phase typically develops one to three weeks following infection from an infected tick bite. During this initial stage, dogs commonly develop high fever ranging from 103-105°F, accompanied by pronounced lethargy and decreased appetite. These early symptoms often prompt concerned owners to seek veterinary attention, creating opportunities for early diagnosis and intervention.
Enlarged lymph nodes, particularly those easily palpated in the neck and behind the knees, represent another hallmark of acute infection. The spleen may also become enlarged, sometimes detectable during physical examination. Many dogs develop respiratory distress, including coughing and exercise intolerance, which may initially suggest heart or lung problems.
Weight loss occurs rapidly during this phase, often accompanied by general depression and reluctance to engage in normal activities. Laboratory testing during the acute stage typically reveals thrombocytopenia-abnormally low platelet counts that can cause minor bleeding tendencies. This phase generally lasts 2-4 weeks, with dogs either progressing to recovery or advancing to the subclinical phase.
Subclinical Phase (weeks to years)
The subclinical phase represents perhaps the most insidious aspect of ehrlichiosis in dogs. During this period, infected dogs show no visible clinical symptoms while the bacterial infection persists within their white blood cells. Dogs can remain persistent subclinical carriers for months or even years, appearing completely healthy to their owners.
Laboratory abnormalities continue during this phase, most notably persistent thrombocytopenia and mild anemia. Veterinarians may notice prolonged bleeding from routine procedures like venipuncture or nail trimming, providing subtle clues to ongoing infection. These subclinically infected dogs pose particular challenges because they can serve as reservoirs for tick infection while appearing perfectly healthy.
The duration of the subclinical phase varies tremendously between individual dogs. Some may remain in this state indefinitely, while others progress to chronic disease when stressed or immunocompromised. Factors triggering progression include concurrent illness, surgical procedures, pregnancy, or other conditions that challenge the immune system.
Chronic Phase (months to years)
Dogs that progress to chronic ehrlichiosis develop severe clinical signs that can become life-threatening without prompt intervention. Severe bleeding disorders characterize this phase, including spontaneous nosebleeds, extensive bruising from minor trauma, and potentially fatal internal hemorrhage.
Profound anemia develops as bone marrow function becomes compromised, often requiring blood transfusions to maintain adequate oxygen-carrying capacity. The bone marrow suppression can progress to pancytopenia, where production of all blood cell types becomes critically impaired.
Neurological symptoms emerge in many chronically infected dogs, including seizures, loss of coordination (ataxia), and significant behavioral changes. These symptoms reflect either direct bacterial effects on the nervous system or secondary complications from severe anemia and bleeding disorders.
Eye problems frequently develop during chronic phases, ranging from retinal hemorrhage and inflammation (uveitis) to complete blindness. Joint pain and lameness may occur, causing dogs to show reluctance to move or exercise.
In advanced cases, kidney damage can progress to renal failure, while immune system dysfunction increases susceptibility to secondary infections. The chronic stage carries a guarded prognosis, with some dogs developing irreversible organ damage despite successful bacterial elimination.
Diagnostic Methods
Accurate diagnosis of canine ehrlichiosis requires combining clinical suspicion with appropriate laboratory testing. The diagnostic approach varies depending on the disease phase and the time elapsed since initial infection.
Initial screening often begins with antibody tests using ELISA technology, commonly performed during routine wellness examinations in endemic areas. These tests detect the immune system's response to ehrlichial infection but may remain negative during early acute infection before antibody development occurs. It is important to note that antibody tests can cross react with antibodies to other Ehrlichia species, such as Ehrlichia canis and Ehrlichia ewingii, which may complicate interpretation of positive results.
Complete blood count (CBC) testing provides crucial diagnostic information, particularly the detection of thrombocytopenia, which occurs in over 90% of infected dogs. Other findings may include anemia, elevated white blood cell counts, and abnormal cell morphology. Blood chemistry panels often reveal elevated globulin levels and may show evidence of kidney or liver involvement.
Polymerase chain reaction (PCR) testing offers the most sensitive method for detecting ehrlichial DNA in peripheral blood, particularly valuable during acute infection when bacterial loads are highest. PCR can also differentiate between different Ehrlichia species, helping guide treatment decisions and prognosis discussions. Diagnostic testing of infected animals is also important for monitoring disease prevalence and implementing control measures.
Direct microscopic examination of a blood smear may occasionally reveal ehrlichial morulae-clusters of bacteria visible within white blood cells. While highly specific when present, these findings occur rarely and require experienced laboratory personnel for accurate identification.
In chronic cases with severe bone marrow involvement, bone marrow biopsy may be necessary to assess cellular infiltration and determine the extent of marrow damage. This invasive procedure helps guide prognosis and treatment intensity decisions.
Urinalysis provides valuable information about kidney involvement and may reveal protein loss that suggests glomerular damage. In dogs with bleeding disorders, urine may contain blood cells indicating internal hemorrhage.
Diagnostic testing often requires combining multiple approaches, as no single test provides perfect sensitivity and specificity across all disease phases. Many veterinarians use both PCR and serology to maximize diagnostic accuracy. It is also essential to consider differential diagnoses, such as infectious cyclic thrombocytopenia and other tick borne diseases, to rule out other conditions with similar clinical signs.


Treatment Protocols
Doxycycline represents the first-line antibiotic treatment for canine ehrlichiosis, administered at doses of 5-10 mg/kg twice daily for a minimum of 28 days. This tetracycline antibiotic effectively penetrates cells where Ehrlichia bacteria reside, making it particularly suited for treating intracellular infections.
For dogs unable to tolerate doxycycline due to gastrointestinal upset or other adverse effects, alternative antibiotics include minocycline or, in severe cases, chloramphenicol. However, doxycycline remains preferred due to its proven efficacy and relatively mild side effect profile.
Treatment duration often requires extension to 6-8 weeks for chronic or severe cases, particularly those with significant bone marrow involvement. The treatment duration depends on initial disease severity, breed predisposition, and clinical response monitoring.
Supportive care plays a crucial role in managing severely affected dogs. Fluid therapy helps maintain hydration and supports kidney function, while anti-nausea medications encourage eating during the recovery period. Nutritional support becomes particularly important for dogs that have lost significant weight during illness.
In severe cases of ehrlichiosis where dogs develop life-threatening anemia or severe bleeding problems, a blood transfusion may be required as a supportive measure. While a blood transfusion can be vital and even life-saving in these critical situations, it does not treat the underlying ehrlichiosis infection itself; antibiotics are still necessary to eliminate the bacteria.
Corticosteroids occasionally are used in specific cases with severe immune-mediated complications, though their use remains controversial due to potential interference with immune function needed to clear the infection.
Monitoring protocols during treatment include weekly blood work to track improvements in blood cell counts and overall clinical response. Most dogs show clinical improvement within 24-72 hours of beginning appropriate antibiotic therapy, though laboratory normalization may take several weeks.
The prognosis varies significantly by disease phase at diagnosis. Dogs treated during acute infection typically achieve excellent outcomes with complete recovery. Chronic ehrlichiosis carries a more guarded prognosis, with some dogs experiencing permanent complications despite successful bacterial elimination.
Prevention Strategies
Year-round tick prevention represents the most effective strategy for protecting dogs from ehrlichiosis, particularly in endemic areas where tick populations remain active throughout most of the year. Modern preventive products offer multiple options to suit different lifestyles and preferences.
Topical spot-on treatments like Advantix II, Frontline Plus, and Bravecto Topical provide effective tick control when applied according to manufacturer directions. These products kill ticks before they can transmit disease, typically within 12-48 hours of attachment. Monthly application schedules ensure consistent protection, though some newer formulations offer extended duration coverage.
Oral chewable preventatives including NexGard, Simparica, Credelio, and Bravecto chews have gained popularity due to their convenience and effectiveness. These systemic treatments circulate through the bloodstream, killing ticks when they feed. The inability to wash off during swimming or bathing represents a significant advantage over topical products.
Long-acting collar options like Seresto provide up to 8 months of tick protection, making them cost-effective for year-round prevention. These collars release active ingredients gradually, maintaining therapeutic levels throughout the wear period.
Daily tick checks remain important even with preventive products, as no prevention method achieves 100% efficacy. Focus attention on common attachment sites including ears, neck, legs, and between toes. Use a systematic approach, running hands over the entire body to detect any attached ticks.
Proper tick removal techniques using fine-tipped tweezers can prevent disease transmission if performed within 24 hours of attachment. Grasp the tick as close to the skin as possible and pull straight out with steady pressure. Avoid twisting or crushing the tick, which may increase infection risk.
Environmental management around homes can reduce tick populations significantly. Regular lawn maintenance, removal of leaf litter and brush piles, and strategic use of approved acaricides help create less hospitable environments for tick survival and reproduction.
Avoiding high-risk areas during peak tick seasons provides additional protection, particularly for dogs with breed predispositions to severe disease. When hiking or camping in wooded areas, stick to maintained trails and avoid tall grass or dense underbrush where ticks concentrate.


Zoonotic Considerations
While dogs cannot directly transmit ehrlichiosis to humans, infected dogs serve as important indicators of environmental risk. The presence of ehrlichial infection in dogs signals that infected ticks exist in the local environment, potentially posing risks to human family members. Human infections can occur in areas where canine ehrlichiosis is present, as infected animals in the environment increase the likelihood of human infections related to tick-borne pathogens.
Human ehrlichiosis occurs through the same tick vectors but typically involves different bacterial species. E. chaffeensis causes human monocytic ehrlichiosis, while E. ewingii can cause human granulocytic ehrlichiosis. These infections produce symptoms similar to canine disease, including fever, headache, and muscle aches, and represent significant forms of human illness due to their clinical impact.
Shared tick exposure represents the primary concern for households with infected dogs. Ticks brought home on pets can potentially attach to human family members, creating indirect transmission pathways. Minimizing human exposure to ticks is essential to reduce the risk of zoonotic disease transmission. This risk emphasizes the importance of comprehensive household tick prevention measures.
Implementing tick prevention strategies that protect both pets and family members creates the most effective disease control approach. Regular yard treatments, personal protective measures during outdoor activities, and prompt tick removal benefit all household members.
Recognition that infected dogs indicate environmental risk helps families make informed decisions about outdoor activities and prevention measures. Areas where dogs have contracted ehrlichiosis require heightened awareness and robust protection protocols for human family members as well.
FAQ
How long after a tick bite does ehrlichiosis develop in dogs?
Clinical symptoms typically appear 1-3 weeks after infection from an infected tick bite, though the incubation period can range from 8-20 days depending on the dog's immune system and the bacterial load transmitted. The acute phase usually develops within this timeframe, but some dogs may progress directly to the subclinical phase without showing obvious acute disease symptoms.
Can dogs recover completely from chronic ehrlichiosis?
While acute ehrlichiosis has an excellent prognosis with proper doxycycline treatment, chronic ehrlichiosis recovery depends on the extent of organ damage that occurred before treatment began. Some dogs may have permanent blood cell abnormalities or organ dysfunction despite successful bacterial elimination. Dogs with bone marrow damage may require months to years for complete recovery, and some may never return to completely normal blood counts.
Do I need to treat my dog if they test positive for ehrlichiosis antibodies but show no symptoms?
Dogs in the subclinical phase with positive antibodies but no clinical signs may not require immediate treatment; however, veterinarians often recommend monitoring with regular blood work and may prescribe antibiotics if blood cell counts are abnormal or if the dog becomes stressed or immunocompromised. The decision typically depends on platelet counts, overall health status, and risk factors for disease progression.
How effective are tick preventatives against ehrlichiosis transmission?
Modern tick preventatives are highly effective when used correctly, killing ticks within 12-48 hours of attachment and significantly reducing the risk of disease transmission, which requires 3-6 hours of tick feeding. However, no prevention method is 100% effective, making regular tick checks still important. Combining preventive products with environmental management and daily inspections provides the most comprehensive protection.
Can indoor dogs get ehrlichiosis?
While indoor dogs have significantly lower risk, they can still be infected if ticks are brought inside on clothing, other pets, or if they have any outdoor exposure during walks, veterinary visits, or brief yard access. Even short outdoor exposure in tick-endemic areas poses some risk. Brown dog ticks, in particular, can establish populations indoors, making even predominantly indoor dogs potentially vulnerable to infection.






