

Key Takeaways
Cancer affects 1 in 3 dogs during their lifetime and is the leading cause of death in dogs over 10 years old
- Cancer affects 1 in 3 dogs during their lifetime and is the leading cause of death in dogs over 10 years old
- Early detection through regular veterinary checkups significantly improves treatment outcomes and survival rates
- Common warning signs include unexplained lumps, weight loss, decreased appetite, lethargy, and persistent wounds that won’t heal
- Modern veterinary oncology offers effective treatments including surgery, chemotherapy, and radiation therapy that can extend quality of life
- Prevention strategies like spaying/neutering, maintaining healthy weight, and limiting UV exposure can reduce cancer risk in some cases
Early detection through regular veterinary checkups significantly improves treatment outcomes and survival rates
Common warning signs include unexplained lumps, weight loss, decreased appetite, lethargy, and persistent wounds that won’t heal
Modern veterinary oncology offers effective treatments including surgery, chemotherapy, and radiation therapy that can extend quality of life
Prevention strategies like spaying/neutering, maintaining healthy weight, and limiting UV exposure can reduce cancer risk in some cases
Cancer remains one of the most feared diagnoses for pet owners, yet understanding this complex disease can empower you to protect your beloved companion. Cancer in dogs has become increasingly recognized as veterinary medicine advances, with sophisticated diagnostic tools and treatment options now available that were unimaginable just decades ago.
The statistics are sobering but important to understand. Roughly the same rate of cancer occurrence affects dogs as humans, with approximately one in three dogs expected to develop cancer during their lifetime. For senior dogs over 10 years of age, this number climbs to nearly 50%, making cancer the leading cause of death in older dogs.
However, these numbers shouldn’t cause despair. Early detection, accurate diagnosis, and appropriate treatment can dramatically improve outcomes for many canine cancers. This comprehensive guide will help you understand the most common types of cancer affecting dogs, recognize warning signs that warrant immediate veterinary attention, and navigate the complex world of cancer treatment options available today.
Introduction to Dog Cancer
Cancer is a leading cause of death in senior dogs, affecting more than half of dogs over the age of 10. According to the American Veterinary Medical Association, cancer is the leading cause of death in dogs beyond middle age, making it a critical concern for pet owners. Certain breeds, such as Golden Retrievers and Bernese Mountain Dogs, are especially prone to developing cancer due to genetic factors. Among the most common cancers seen in dogs are mast cell tumors, which frequently appear as skin tumors; lymphoma, which targets the lymphatic system; and osteosarcoma, the most common primary bone tumor in dogs, particularly affecting large and giant breeds.
Treating cancer in dogs requires a comprehensive and individualized approach. Options may include surgery to remove tumors, radiation therapy to target cancerous cells, and chemotherapy to address cancers that have spread or are not amenable to surgery. Veterinary oncologists are specialists trained in diagnosing and treating cancer in dogs, and they work closely with pet owners to develop the most effective treatment plan for each case. Early detection and collaboration with veterinary professionals are key to improving outcomes and maintaining quality of life for dogs facing cancer.
Most Common Types of Cancer in Dogs
Understanding the landscape of canine cancers helps pet owners recognize patterns and risk factors specific to their dogs. Over 50% of dogs over 10 years old face a cancer diagnosis, making awareness of common cancer types essential for early intervention.
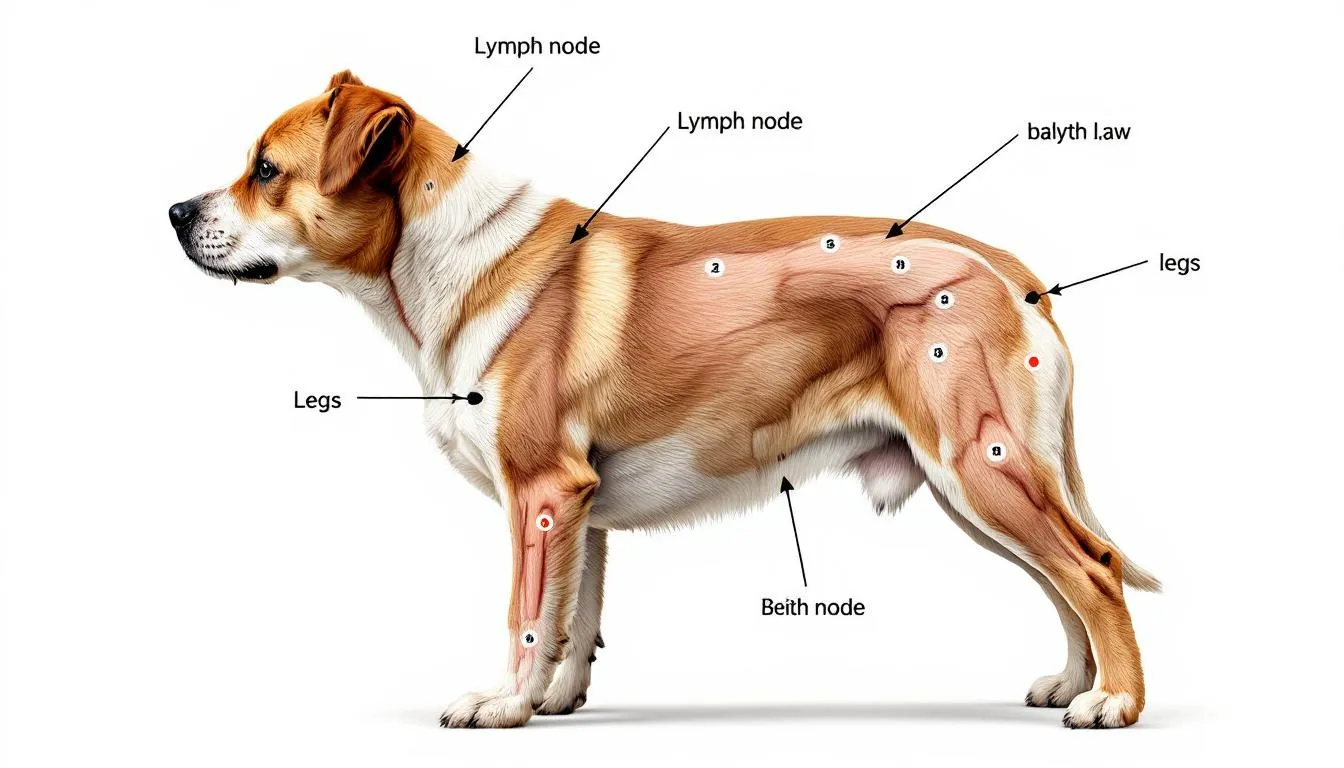
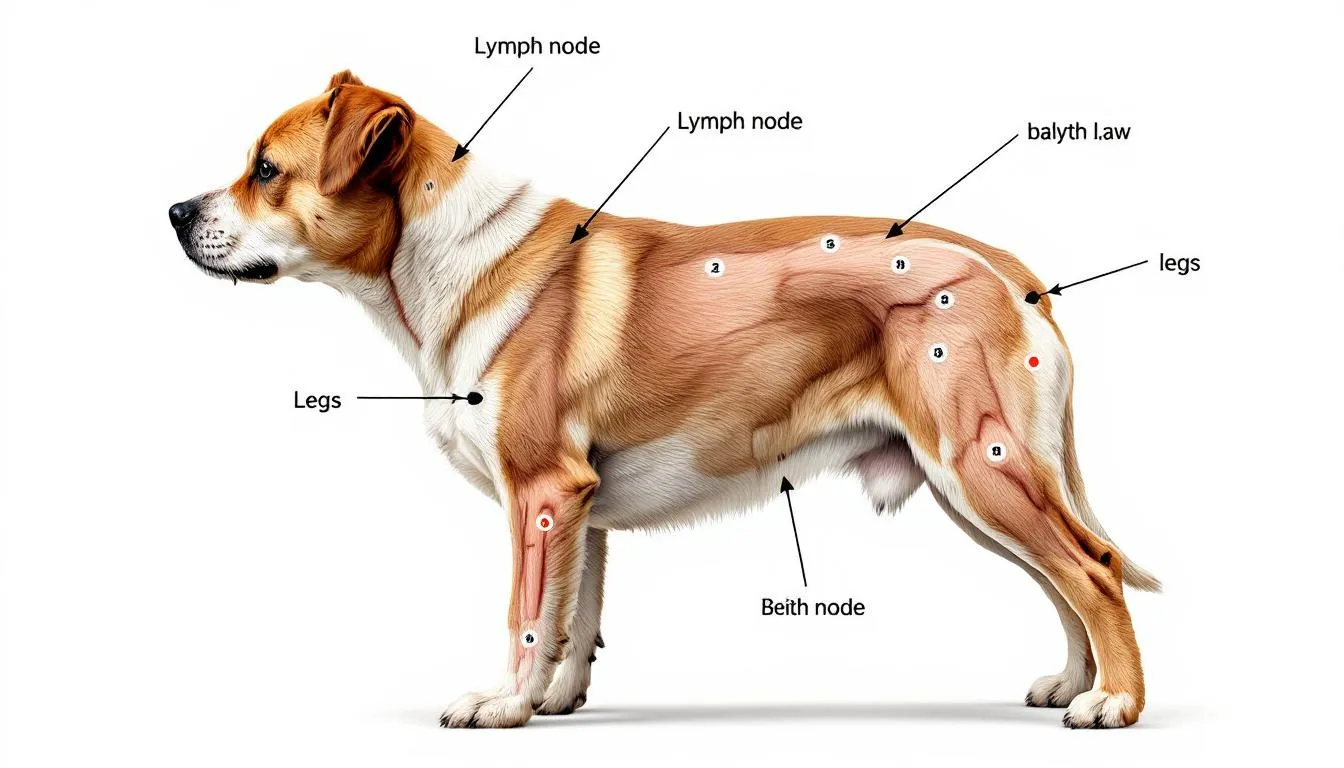
Lymphoma represents one of the most frequently encountered canine cancers, affecting up to 24% of all cancer cases in dogs. Lymphomas are among the most frequently encountered blood or immune-related cancers in dogs. This cancer primarily targets the lymphatic system, with the most common form involving external lymph nodes, particularly in the neck, behind the knees, or in front of the shoulders. Pet owners often first notice swollen lymph nodes during routine petting or grooming. Lymphoma responds well to chemotherapy protocols, with many dogs achieving remission periods of 12-18 months.
Mast cell tumors claim the distinction of being the most common skin cancer in dogs, accounting for approximately 20% of all skin tumors. These tumors require microscopic examination for accurate grading, as their appearance can vary dramatically from small, benign-looking bumps to large, ulcerated masses. The grading system helps veterinary oncologists determine treatment approaches and prognosis.
Osteosarcoma presents as a highly aggressive bone cancer making up 85% of skeletal tumors in dogs. This cancer particularly affects large breed dogs and giant breeds, with the common primary bone tumor typically developing in the long bones of the legs. The affected bone often becomes painful and may fracture easily, leading to sudden lameness in previously healthy dogs.
Hemangiosarcoma develops from blood vessels and represents one of the most challenging canine cancers to treat. These malignant tumors often remain hidden within internal organs like the spleen, liver, and heart until they rupture or cause severe symptoms. The poor prognosis associated with hemangiosarcoma stems from its tendency for distant metastasis before detection.
Melanoma commonly appears as malignant oral tumors that can invade tissue and metastasize rapidly. While skin melanomas in dogs are often benign, oral melanomas are typically malignant and aggressive. These tumors frequently develop on the gums, tongue, or roof of the mouth.
Transitional cell carcinoma affects the urinary system as the most common cancer of the bladder and urethra. This cancer commonly affects middle-aged to older dogs, with breeds such as Scottish Terriers, Shetland Sheepdogs, and Beagles being commonly affected. It can cause symptoms similar to urinary tract infections, often leading to delayed diagnosis.
Tumors of the mammary glands occur more commonly in unspayed females, with hormonal factors playing a significant role in development. The mammary glands are the tissue involved, and approximately 50% of mammary tumors in dogs are malignant, though early surgical removal often provides excellent outcomes for localized tumors.


Recognizing Cancer Symptoms in Dogs
Early recognition of cancer symptoms can mean the difference between successful treatment and advanced disease. Cancer cells can develop anywhere in the body, making symptom awareness crucial for all pet owners.
Physical symptoms often provide the first clues to cancer presence. Unexplained lumps or bumps anywhere on the body warrant immediate veterinary evaluation, as visual examination alone cannot distinguish between benign and malignant masses. Swollen lymph nodes, particularly those under the jaw, in front of the shoulders, or behind the knees, may indicate lymphoma or metastatic disease. Abnormal bleeding or discharge from any body opening, including the mouth, nose, ears, or urogenital areas, requires prompt investigation.
Behavioral changes frequently accompany cancer development as the disease affects your dog’s overall well-being. Decreased appetite often appears as one of the earliest signs, sometimes weeks before other symptoms become apparent. Significant weight loss, especially when accompanied by maintained or increased appetite, may indicate metabolic changes associated with cancer. Lethargy and reduced activity levels can signal pain or systemic illness, while difficulty eating or swallowing suggests oral or throat involvement.
Respiratory signs become particularly important when cancer affects the chest cavity or spreads to the lungs. Persistent coughing, especially when accompanied by exercise intolerance, may indicate lung involvement or heart-based tumors. Labored breathing or rapid respiratory rate at rest warrants immediate veterinary attention.
Neurological symptoms can indicate brain tumors or cancers that have metastasized to the nervous system. Seizures in dogs without a previous history, balance problems, or sudden behavioral changes may signal central nervous system involvement requiring urgent evaluation.
Wound healing issues often accompany certain cancer types, particularly skin tumors. Sores that don’t heal within a reasonable timeframe, persistent infections, or pale gums indicating anemia all require professional assessment.
Location-specific symptoms help narrow diagnostic possibilities. Limping or sudden onset lameness may indicate bone cancer, particularly in large breed dogs. Urinary issues including frequent urination, blood in urine, or straining may suggest bladder cancer. Excessive drooling, bad breath, or difficulty chewing can indicate oral tumors.
Pet owners should seek immediate veterinary attention for any new lump or sudden behavioral change, as early intervention significantly improves treatment outcomes for most canine cancers.
Understanding Cancer Causes and Risk Factors
Cancer development in dogs results from multiple factors working together over time, with age-related factors playing the most significant role. Cancer risk increases substantially after 7-10 years of age as cellular repair mechanisms become less efficient and DNA damage accumulates throughout the body.
Genetic predisposition creates varying cancer risks among different breeds. Certain breeds like Golden Retrievers, Boxers, German Shepherds, and Bernese Mountain Dogs demonstrate significantly higher cancer rates compared to mixed breeds. Golden Retrievers face particularly elevated risks for lymphoma and hemangiosarcoma, while Boxers show increased susceptibility to mast cell tumors. Large and giant breeds carry higher risks for osteosarcoma compared to smaller dogs.
Environmental triggers contribute to cancer development through various pathways. UV radiation exposure increases skin cancer risks, particularly in light-colored or hairless breeds. Chemical toxins, pesticides, and environmental pollutants can cause DNA damage leading to malignant transformation. Chronic exposure to secondhand smoke has been linked to certain canine cancers, similar to human exposure patterns.
Viral and infectious causes play roles in specific cancer types, though less commonly than in human cancers. Some cancers show associations with viral infections or chronic inflammatory conditions that create cellular stress over extended periods.
Hormonal influences significantly impact cancer development, particularly for mammary gland tumors. Unspayed females face dramatically higher mammary cancer risks, with the risk dropping to less than 0.5% if spaying occurs before the first heat cycle. Male dogs also benefit from neutering, which reduces testicular cancer risks.
The development of cancerous cells typically requires multiple genetic “hits” occurring over time, explaining why cancer incidence increases with age. DNA mutations accumulate throughout life due to normal cellular processes, environmental exposures, and oxidative stress. When cellular repair mechanisms can no longer maintain genetic integrity, malignant transformation may occur.
Understanding that cancer typically results from the interaction of multiple factors helps explain why prevention strategies focus on reducing controllable risk factors while acknowledging that some factors, like genetics and age, cannot be modified.
Identifying Cancerous Lumps vs. Normal Masses
Pet parents frequently discover lumps during routine petting or grooming, creating anxiety about potential cancer. Understanding the characteristics that distinguish concerning masses from benign growths helps guide appropriate responses.
Visual characteristics of cancerous lumps vary greatly, making professional evaluation essential. Malignant tumors can present as small, seemingly innocent bumps or large, obvious masses. Size alone doesn’t determine malignancy, as some aggressive cancers begin as tiny nodules while some large masses remain benign. Texture variations include soft, firm, or rock-hard consistency, with none being definitively diagnostic.
Growth patterns provide more reliable indicators of concern. Rapid growth over days to weeks often suggests malignancy, though some benign masses can also grow quickly. Irregular borders or asymmetrical shapes raise suspicion compared to smooth, round masses. However, many malignant tumors present with regular borders, making visual assessment unreliable.
Location significance influences cancer probability, with lymph nodes representing important monitoring sites. Lymph nodes are small, oval-shaped swellings located in predictable anatomical locations that can enlarge with infection, inflammation, or cancer. Common sites include under the jaw, in front of the shoulders, behind the knees, and in the groin area.
Mobility factors traditionally suggested that fixed masses attached to underlying tissues were more concerning than moveable lumps. While this remains somewhat true, many malignant tumors remain freely moveable, particularly in early stages.
Associated symptoms provide crucial context for lump evaluation. Masses accompanied by bleeding, ulceration, pain, or rapid size changes require immediate evaluation regardless of other characteristics. Tumor size can significantly affect clinical signs, with larger tumors more likely to cause noticeable swelling, pain, and increase the risk of complications such as fractures. Systemic symptoms like lethargy, decreased appetite, or weight loss in conjunction with new lumps heighten concern levels.
The critical message for pet owners remains that visual diagnosis proves unreliable for distinguishing benign from malignant masses. Any new lump discovered during routine handling should prompt veterinary evaluation, particularly in dogs over 7 years of age or breeds with known cancer predispositions.
Veterinary Diagnosis Methods and Advanced Testing
Modern veterinary medicine employs sophisticated diagnostic approaches that mirror human oncology practices. The journey from initial lump discovery to definitive cancer diagnosis involves multiple steps, each providing crucial information for treatment planning.
Initial physical examination forms the foundation of cancer diagnosis, with experienced veterinarians conducting comprehensive assessments for lumps, masses, and organ enlargement. A thorough physical exam includes palpation of all accessible lymph nodes, abdominal organs, and careful oral examination. Veterinarians diagnose cancer through systematic evaluation, but definitive diagnosis requires additional testing. Examples of additional tests include CT scans, bone marrow aspirates, or additional biopsies to further determine the extent and stage of the cancer.
Fine needle aspirate (FNA) represents the first-line diagnostic tool for accessible masses. This minimally invasive procedure involves inserting a small needle into the tumor to collect cells for microscopic examination. FNA can often distinguish between inflammatory conditions, benign tumors, and malignant processes, though it may not provide complete information about tumor grade or subtype.
Surgical biopsy provides definitive tissue sampling when FNA results are inconclusive or when complete tumor characterization is necessary. This procedure removes a portion or the entire mass for comprehensive histopathological examination, allowing pathologists to determine exact tumor type, grade, and margins if completely excised.
Blood work analysis includes complete blood counts, comprehensive chemistry panels, and specialized tests. Blood tests can reveal anemia, abnormal protein levels, or organ dysfunction that might influence treatment decisions. While most cancers don’t cause specific blood test abnormalities, some types like lymphoma may show characteristic changes.
Advanced imaging techniques have revolutionized cancer diagnosis and staging. X-rays remain essential for evaluating chest and bone involvement, particularly important for detecting lung metastasis or primary bone tumors. Ultrasound examination provides detailed evaluation of abdominal organs, allowing assessment of internal organ involvement and guidance for additional sampling procedures. Further testing may be recommended after these imaging studies to determine the extent and stage of the cancer.
Specialized scans including CT scans offer detailed cross-sectional imaging for precise tumor localization and surgical planning. Magnetic resonance imaging (MRI) excels at evaluating soft tissue detail and brain involvement, though requiring general anesthesia for proper positioning.
Cancer staging procedures determine the extent of disease spread, crucial for prognosis and treatment selection. Staging typically involves imaging studies to detect metastasis, lymph node evaluation, and sometimes bone marrow aspirates for blood-related cancers.
The American Veterinary Medical Association emphasizes that accurate diagnosis requires professional expertise and appropriate testing, as treatment success depends heavily on understanding exactly what type of cancer is present and how far it has spread. A veterinary oncologist may be consulted for specialized diagnostic procedures and to develop a comprehensive treatment plan tailored to the individual patient.
Diagnostic Imaging in Canine Cancer
Diagnostic imaging is a cornerstone of cancer diagnosis and management in dogs, providing veterinarians with detailed insights into the presence, location, and extent of tumors. Advanced imaging techniques such as computed tomography (CT) scans and magnetic resonance imaging (MRI) allow for precise visualization of internal organs and tissues, which is essential for accurate cancer diagnosis and staging. CT scans are particularly valuable for detecting tumors in the chest and abdomen, helping veterinarians identify masses that may not be palpable during a physical exam. MRI is especially useful for evaluating tumors affecting the brain and spinal cord, offering high-resolution images that guide treatment planning.
In addition to imaging, fine needle aspirate procedures and biopsies are commonly used to obtain tissue samples from suspected tumors. These samples are then examined under a microscope to determine the type of cancer and its characteristics. Blood tests, including complete blood counts and chemistry profiles, provide important information about the dog’s overall health and can reveal abnormalities that may be associated with cancer. Early detection through advanced imaging and laboratory testing is critical for successful treatment, as it allows for timely intervention and more effective management of the disease.
Staging and Grading of Canine Tumors
Staging and grading are essential steps in the evaluation of canine tumors, guiding both prognosis and treatment decisions. Staging refers to determining how far the cancer has spread within the body. This process involves assessing the size of the tumor, checking for involvement of nearby lymph nodes, and identifying any distant metastasis to other organs. Accurate staging often relies on a combination of advanced imaging, such as CT scans or MRI, and diagnostic procedures like fine needle aspirate or biopsy.
Grading, on the other hand, focuses on the microscopic appearance of the tumor cells. Using systems like the World Health Organization (WHO) grading scale, pathologists classify tumors based on how closely the cancer cells resemble normal tissue and how rapidly they are dividing. Tumors are typically graded from I (low grade) to III (high grade), with high grade tumors being more aggressive and associated with a poorer prognosis.
Veterinary oncologists use the information from staging and grading to develop a tailored treatment plan and to provide pet owners with an accurate understanding of what to expect. This comprehensive approach ensures that each dog receives the most appropriate care, maximizing the chances for successful treatment and maintaining the best possible quality of life.


Treatment Options and Modern Veterinary Oncology
Veterinary oncology has evolved dramatically over the past two decades, offering treatment options that can significantly extend both survival time and quality of life for dogs with cancer. Treatment depends entirely on tumor type, stage, location, and the individual dog’s overall health status. Veterinary oncologists use a combination of therapies to treat cancer in dogs, including surgery, chemotherapy, and radiation.
Surgical intervention remains the cornerstone of cancer treatment for many tumor types. Complete surgical removal can be curative for localized cancers when adequate margins are achieved. For bone cancers like osteosarcoma, aggressive surgery including limb amputation often provides the best chance for extended survival. Debulking procedures, which remove most but not all tumor tissue, can improve quality of life even when cure isn’t possible.
Chemotherapy protocols in veterinary medicine differ significantly from human treatments, focusing on maintaining quality of life while controlling disease. Common drugs include doxorubicin, carboplatin, vincristine, and prednisone, often used in specific combinations proven effective for particular cancer types. Veterinary oncologists carefully adjust dosages to minimize side effects while maintaining therapeutic benefit.
Radiation therapy provides targeted treatment for localized tumors that cannot be completely surgically removed or for cancers in locations where surgery would be too invasive. This treatment option is often combined with surgery to improve local control and reduce recurrence risk.
Immunotherapy approaches represent newer treatments that stimulate the immune system to recognize and attack cancer cells. While still evolving in veterinary medicine, these treatments show promise for certain cancer types and are available through specialized cancer centers.
Palliative care options focus on maintaining comfort and quality of life when curative treatment isn’t possible or appropriate. This approach emphasizes pain management, nutritional support, and addressing symptoms that impact daily activities. Many dogs can maintain excellent quality of life for extended periods with well-managed palliative care.
Integrated treatment plans combining multiple modalities often provide optimal outcomes. For example, surgical removal followed by chemotherapy, or radiation therapy combined with surgical debulking, can extend survival beyond what any single treatment might achieve.
Several FDA-approved cancer drugs specifically designed for veterinary use have expanded treatment options. These medications undergo rigorous testing for safety and efficacy in dogs, providing veterinarians with proven therapeutic tools.
Clinical trials and experimental treatments through specialized cancer centers offer additional options for dogs with difficult-to-treat cancers. These programs often provide access to cutting-edge therapies while contributing to advancement in veterinary oncology.
Managing Treatment Side Effects and Quality of Life
Successful cancer treatment in dogs requires careful attention to side effects and continuous quality of life assessment. Unlike human chemotherapy, veterinary protocols prioritize maintaining normal daily activities and minimizing discomfort throughout treatment.
Common chemotherapy side effects in dogs include decreased appetite, mild lethargy, and occasional gastrointestinal upset. Bone marrow suppression can occur, temporarily reducing white blood cell counts and increasing infection risk. Most dogs tolerate chemotherapy remarkably well, with severe side effects being uncommon when protocols are properly managed.
Monitoring protocols include regular blood work to assess organ function and blood cell counts, physical examinations to evaluate treatment response, and careful owner observations of daily activities. Pet owners play crucial roles in reporting changes in appetite, energy levels, or behavior that might indicate treatment adjustments are needed.
Supportive care measures help minimize side effects and maintain comfort. Anti-nausea medications can prevent chemotherapy-induced nausea, while nutritional support ensures adequate caloric intake during treatment. Infection prevention becomes important during periods of immune suppression, requiring careful attention to wound care and environmental exposures.
Quality of life assessment tools help guide treatment decisions by objectively evaluating mobility, appetite, interaction with family, and overall enjoyment of daily activities. Many veterinary oncologists use standardized scoring systems to track changes over time and determine when treatment modifications might be beneficial.
Communication with the veterinary team proves essential for optimal outcomes. Pet owners should report any concerning changes promptly, as early intervention can often prevent minor side effects from becoming serious problems. Regular check-ins allow for treatment adjustments based on individual responses.
Treatment modification strategies ensure that therapy remains appropriate for each individual dog. Dose reductions, schedule changes, or drug substitutions can maintain therapeutic benefit while reducing side effects. The goal remains controlling cancer while preserving the human-animal bond and daily quality of life.
End-of-life considerations require honest discussions about treatment goals, prognosis, and quality of life expectations. Veterinary teams help families navigate difficult decisions about when to continue aggressive treatment versus transitioning to comfort-focused care.
The fundamental difference between cure-focused and comfort-focused treatment approaches lies in the primary goal: cure-focused treatments aim to eliminate cancer even if temporary discomfort results, while comfort-focused approaches prioritize immediate quality of life and symptom management.


Prevention Strategies and Risk Reduction
While not all canine cancers can be prevented, several evidence-based strategies can significantly reduce risk for many cancer types. Prevention efforts focus on modifying controllable risk factors while maintaining overall health and immune system function.
Spaying and neutering benefits extend beyond population control to include substantial cancer risk reduction. Spaying female dogs before their first heat cycle reduces mammary cancer risk to less than 0.5%, compared to 25% risk in intact females. Neutering males eliminates testicular cancer risk and reduces prostate disease, though timing recommendations may vary based on breed size and other health considerations.
Regular veterinary checkups enable early detection when treatment outcomes are most favorable. Annual examinations for adult dogs and bi-annual visits for senior dogs over 7 years allow veterinarians to detect changes before they become advanced. These routine checkups should include thorough physical examinations, palpation of all accessible areas, and discussion of any owner concerns.
UV protection measures become particularly important for light-colored breeds, hairless varieties, and dogs with thin coat coverage. Limiting sun exposure during peak hours, providing shaded outdoor areas, and considering protective clothing for susceptible dogs can reduce skin cancer risks.
Maintaining healthy body weight through proper diet and exercise provides multiple health benefits including potential cancer risk reduction. Obesity creates chronic inflammatory conditions that may contribute to cancer development, while appropriate body condition supports optimal immune function.
Environmental toxin avoidance involves reducing exposure to known carcinogens when possible. This includes minimizing pesticide and herbicide exposure, avoiding secondhand smoke, and being cautious with household chemicals. While complete avoidance isn’t always practical, awareness helps pet owners make informed decisions about their dog’s environment.
Breed-specific screening recommendations help identify cancers early in genetically predisposed dogs. Breeds with known cancer risks may benefit from more frequent examinations, specialized screening tests, or earlier implementation of preventive measures.
Home monitoring techniques empower pet owners to detect changes early. Regular “hands-on” examinations during grooming or petting can identify new lumps or changes in existing masses. Establishing baseline knowledge of your dog’s normal anatomy helps recognize deviations that warrant professional evaluation.
Vaccination protocols to prevent virus-associated cancers remain important, though viral causes are less common in dogs than in some other species. Maintaining current vaccinations supports overall immune health and prevents diseases that might compromise cancer surveillance mechanisms.
Cost Considerations and Financial Planning
Cancer treatment costs represent a significant concern for many pet families, with expenses varying dramatically based on cancer type, stage, and chosen treatment approach. Understanding financial implications helps families make informed decisions aligned with their resources and treatment goals.
Treatment cost ranges span from hundreds of dollars for simple surgical removals to over $15,000 for comprehensive protocols involving surgery, chemotherapy, and radiation therapy. Diagnostic procedures including advanced imaging, biopsies, and staging studies typically cost $1,000-3,000 before treatment begins.
Factors affecting costs include diagnostic complexity, surgical requirements, chemotherapy protocols, and radiation therapy needs. Geographic location significantly influences pricing, with specialty centers in urban areas typically charging more than general practice treatments. The specific cancer type also impacts costs, as some require more intensive monitoring or expensive medications.
Pet insurance coverage options vary widely in cancer treatment coverage, with many policies excluding pre-existing conditions. Pet owners should carefully review policy details regarding cancer coverage, annual limits, and lifetime maximums. Some policies cover experimental treatments while others limit coverage to conventional therapies.
Lower-cost treatment alternatives may be available through veterinary schools, where supervised students provide care at reduced rates. Some general practitioners offer chemotherapy administration, potentially reducing costs compared to specialist referral. Palliative care approaches often cost significantly less than aggressive treatment protocols while still providing quality of life benefits.
Clinical trial participation opportunities sometimes provide access to experimental treatments at reduced cost or no charge to owners. Research institutions conducting cancer studies may offer cutting-edge therapies while gathering data on treatment effectiveness.
Financial assistance programs exist through various veterinary organizations, breed clubs, and charitable foundations. These programs may provide grants or low-interest loans for cancer treatment, though application processes and eligibility requirements vary.
Cost-benefit analysis should consider prognosis, expected quality of life, and family financial capacity. A $5,000 treatment providing six months of good quality life might be worthwhile for some families but inappropriate for others facing financial hardship.
Planning discussions with the veterinary team about budget constraints and treatment priorities help ensure that chosen approaches align with both medical possibilities and financial realities. Many veterinarians can suggest modified protocols that provide benefits at reduced costs.
FAQ
How long can dogs live with cancer after diagnosis?
Survival time varies dramatically depending on cancer type, stage at diagnosis, and treatment approach. Dogs with lymphoma receiving chemotherapy often live 12-24 months, while those with osteosarcoma may survive 6-18 months with aggressive treatment including amputation and chemotherapy. Hemangiosarcoma typically carries a prognosis of 2-6 months even with treatment, while completely excised mast cell tumors may result in normal life expectancy. Early detection and appropriate treatment significantly improve outcomes across all cancer types.
Can cancer be completely cured in dogs?
Yes, many canine cancers can be cured with appropriate treatment, particularly when detected early. Completely excised low-grade mast cell tumors, early-stage mammary tumors, and some skin cancers often result in cure. However, some aggressive cancer types like hemangiosarcoma and high-grade tumors are rarely curable, though treatment can significantly extend quality life. The concept of “cure” in veterinary oncology often means long-term disease-free survival rather than guaranteed permanent elimination.
Are certain dog breeds more prone to specific types of cancer?
Genetic predisposition plays a significant role in cancer development, with certain breeds showing dramatically higher risks for specific cancer types. Golden Retrievers face elevated risks for lymphoma and hemangiosarcoma, Boxers commonly develop mast cell tumors, and large breeds like Great Danes have increased osteosarcoma risk. Bernese Mountain Dogs show high overall cancer rates, while Scottish Terriers are prone to bladder cancer. Understanding breed predispositions helps with early screening and prevention strategies.
What should I do if I find a new lump on my dog?
Any new lump should be evaluated by a veterinarian promptly, regardless of size or appearance. Schedule an appointment within a few days for non-urgent lumps, or immediately if the mass is rapidly growing, bleeding, or causing pain. Avoid “wait and see” approaches, as early diagnosis significantly improves treatment outcomes. Document the lump with photos and note any changes in size or characteristics while waiting for the appointment.
How do I know if my dog is suffering during cancer treatment?
Quality of life assessment focuses on your dog’s ability to enjoy normal activities like eating, playing, and interacting with family. Warning signs of poor quality of life include persistent loss of appetite, inability to stand or walk comfortably, difficulty breathing, or withdrawal from family interaction. Most dogs receiving appropriate veterinary oncology care maintain good quality of life throughout treatment, as protocols are designed to minimize side effects while controlling disease. Regular communication with your veterinary team helps ensure treatment adjustments maintain comfort.
FAQ
How long can dogs live with cancer after diagnosis?
Survival time varies dramatically depending on cancer type, stage at diagnosis, and treatment approach. Dogs with lymphoma receiving chemotherapy often live 12-24 months, while those with osteosarcoma may survive 6-18 months with aggressive treatment including amputation and chemotherapy. Hemangiosarcoma typically carries a prognosis of 2-6 months even with treatment, while completely excised mast cell tumors may result in normal life expectancy. Early detection and appropriate treatment significantly improve outcomes across all cancer types.
Can cancer be completely cured in dogs?
Yes, many canine cancers can be cured with appropriate treatment, particularly when detected early. Completely excised low-grade mast cell tumors, early-stage mammary tumors, and some skin cancers often result in cure. However, some aggressive cancer types like hemangiosarcoma and high-grade tumors are rarely curable, though treatment can significantly extend quality life. The concept of “cure” in veterinary oncology often means long-term disease-free survival rather than guaranteed permanent elimination.
Are certain dog breeds more prone to specific types of cancer?
Genetic predisposition plays a significant role in cancer development, with certain breeds showing dramatically higher risks for specific cancer types. Golden Retrievers face elevated risks for lymphoma and hemangiosarcoma, Boxers commonly develop mast cell tumors, and large breeds like Great Danes have increased osteosarcoma risk. Bernese Mountain Dogs show high overall cancer rates, while Scottish Terriers are prone to bladder cancer. Understanding breed predispositions helps with early screening and prevention strategies.
What should I do if I find a new lump on my dog?
Any new lump should be evaluated by a veterinarian promptly, regardless of size or appearance. Schedule an appointment within a few days for non-urgent lumps, or immediately if the mass is rapidly growing, bleeding, or causing pain. Avoid “wait and see” approaches, as early diagnosis significantly improves treatment outcomes. Document the lump with photos and note any changes in size or characteristics while waiting for the appointment.
How do I know if my dog is suffering during cancer treatment?
Quality of life assessment focuses on your dog’s ability to enjoy normal activities like eating, playing, and interacting with family. Warning signs of poor quality of life include persistent loss of appetite, inability to stand or walk comfortably, difficulty breathing, or withdrawal from family interaction. Most dogs receiving appropriate veterinary oncology care maintain good quality of life throughout treatment, as protocols are designed to minimize side effects while controlling disease. Regular communication with your veterinary team helps ensure treatment adjustments maintain comfort.






