Key Takeaways
- Anemia occurs when dogs have insufficient red blood cells or hemoglobin, often indicating an underlying health condition rather than being a standalone disease
- Common symptoms include pale gums, weakness, lethargy, rapid breathing, and increased heart rate, with severity varying based on the underlying cause
- Three main types exist: blood loss anemia (from injury or internal bleeding), hemolytic anemia (destruction of red blood cells), and non-regenerative anemia (insufficient production)
- Treatment focuses on addressing the root cause, which may include medications, blood transfusions, immune suppression, or surgical intervention depending on the diagnosis
- Prevention involves year-round parasite control, avoiding toxic substances, maintaining a healthy diet, and regular veterinary wellness exams for early detection
Anemia occurs when dogs have insufficient red blood cells or hemoglobin, often indicating an underlying health condition rather than being a standalone disease
Common symptoms include pale gums, weakness, lethargy, rapid breathing, and increased heart rate, with severity varying based on the underlying cause
Three main types exist: blood loss anemia (from injury or internal bleeding), hemolytic anemia (destruction of red blood cells), and non-regenerative anemia (insufficient production)
Treatment focuses on addressing the root cause, which may include medications, blood transfusions, immune suppression, or surgical intervention depending on the diagnosis
Prevention involves year-round parasite control, avoiding toxic substances, maintaining a healthy diet, and regular veterinary wellness exams for early detection


What is Anemia in Dogs?
When your dog’s energy suddenly drops and their gums appear pale, anemia in dogs might be the underlying cause. Anemia represents a clinical condition characterized by a decrease in circulating red blood cells, hemoglobin concentration, or both, which significantly reduces the blood’s oxygen-carrying capacity throughout the dog’s body.
Understanding that anemia serves as a symptom of underlying disease rather than a standalone condition is crucial for proper management. Anemia in dogs results from another disease process or condition that affects red blood cell production, destruction, or loss. The red blood cell lifecycle typically spans approximately three months before these cells are naturally recycled by the spleen and bone marrow. When this delicate balance becomes disrupted, developing anemia occurs through three primary mechanisms: decreased red blood cell production in the bone marrow, increased destruction of existing red blood cells, or blood loss from the circulatory system.
Dogs anemia occurs when the body does not produce enough red blood cells, destroys them too quickly, or loses them through bleeding. The bone marrow normally produces new red blood cells at a rate that maintains adequate oxygen delivery to tissues. However, when the bone marrow responds inappropriately or cannot produce enough red blood cells to meet the body’s demands, the resulting oxygen deficit creates the clinical signs associated with this serious condition.
Developing Anemia in Dogs
Anemia in dogs doesn’t happen overnight—it’s often the result of complex processes that disrupt the balance of red blood cells in your dog’s body. One of the most common causes is immune mediated hemolytic anemia, where the immune system mistakenly targets and destroys healthy red blood cells. This can be triggered by certain genetic disorders, infections, or even exposure to toxins. In other cases, developing anemia may stem from blood loss anemia, which occurs after severe blood loss due to trauma, surgery, or internal bleeding from conditions like stomach ulcers or cancer. Some dogs are born with genetic disorders that make their red blood cells more fragile or prone to destruction, increasing their risk of developing anemia over time. Recognizing these risk factors and understanding how blood cells are affected by the immune system or by internal bleeding is key to catching anemia early and seeking prompt veterinary care.
Recognizing Symptoms of Anemia in Dogs
Early recognition of anemia symptoms can significantly improve treatment outcomes for affected dogs. The most reliable indicator remains pale gums, which should normally appear a healthy pink color. When red blood cell count drops, these mucous membranes lose their vibrant coloration, appearing white, gray, or even bluish in severe cases.
Primary symptoms include progressive weakness that may initially appear as reluctance to exercise or climb stairs. Dogs often display increased lethargy, spending more time resting and showing decreased interest in activities they previously enjoyed. Rapid breathing, even at rest, develops as the dog’s body attempts to compensate for reduced oxygen-carrying capacity.
Secondary signs manifest as the condition progresses. Increased heart rate occurs as the cardiovascular system works harder to circulate the available red blood cells more efficiently. Loss of appetite frequently accompanies the general malaise, while low blood pressure may develop in more severe cases.
In acute situations, particularly those involving rapid blood loss or severe hemolytic anemia, dogs may experience jaundice (yellowing of the gums and whites of the eyes), shock, and even collapse. These emergency symptoms require immediate veterinary intervention, as they indicate life-threatening complications that can progress rapidly without proper treatment.
Types of Anemia in Dogs
Blood loss anemia develops when dogs lose significant amounts of blood either acutely or chronically. Acute blood loss typically results from trauma, surgical complications, or a bleeding disorder that causes rapid hemorrhage. When severe loss of blood exceeds 30-40% of total blood volume, emergency treatment becomes necessary to prevent shock and death.
Blood Loss Anemia
Chronic blood loss presents more subtly, often developing over weeks or months through sources like stomach ulcers, gastrointestinal tumors, or persistent parasite infestations. Internal bleeding from these conditions gradually depletes the body’s iron stores, eventually leading to iron deficiency anemia. This type often goes unrecognized initially because dogs adapt to the gradual decrease in red blood cell count.
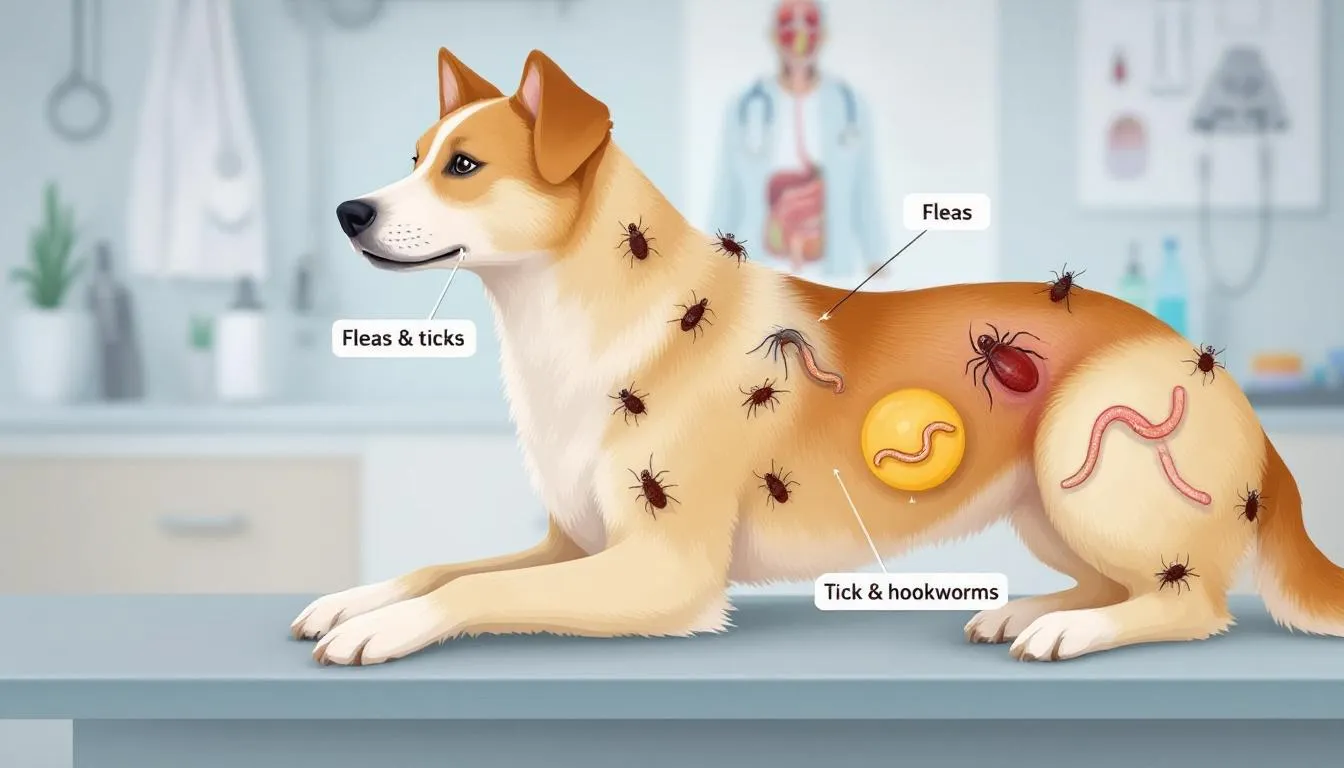
Internal parasites, particularly hookworms and heavy flea infestations, represent common causes of chronic blood loss in dogs. These blood-sucking parasites can drain significant amounts of blood over time, especially in puppies or smaller dogs where even modest blood loss has greater impact.
The bone marrow typically responds appropriately to blood loss anemia by increasing red blood cell production, making this a regenerative anemia. However, when iron deficiency develops from chronic blood loss, the bone marrow’s ability to produce healthy red blood cells becomes compromised despite adequate stimulation.
Hemolytic Anemia
Hemolytic anemia occurs when red blood cells are destroyed faster than the bone marrow can replace them. Immune mediated hemolytic anemia represents the most common form in dogs, where the immune system mistakenly identifies the dog’s own red blood cells as foreign invaders and destroys them.
Autoimmune hemolytic anemia can develop as a primary condition or secondary to other factors including infections, certain medications, vaccinations, or tumors. This condition carries significant risks beyond simple anemia, as the destruction of red blood cells can trigger dangerous blood clots in small blood vessels throughout the brain and lungs. In severe cases, this may progress to disseminated intravascular coagulation (DIC), a serious condition characterized by widespread intravascular coagulation and depletion of essential clotting components.
Secondary causes of hemolytic anemia include various infections such as Babesia and Ehrlichia transmitted through tick bites. Toxic substances like acetaminophen, onions, garlic, and zinc can also trigger red blood cell destruction. Even some medications, including certain antibiotics and chemotherapy drugs, may cause hemolytic reactions in susceptible dogs.
The rapid destruction of red blood cells in hemolytic anemia often produces additional symptoms beyond typical anemia signs. Dogs may develop jaundice as the liver processes the excess hemoglobin released from destroyed cells, and their urine may appear dark red or brown due to hemoglobin spillover into the kidneys.
Non-Regenerative Anemia
Non regenerative anemia develops when the bone marrow fails to produce adequate red blood cells despite appropriate stimulation. This type indicates insufficient production at the cellular level, often due to bone marrow disease, chronic illness, or systemic conditions affecting blood forming cells.
Kidney disease represents a leading cause of non-regenerative anemia in dogs. The kidneys produce erythropoietin, a hormone that stimulates red blood cell production in the bone marrow. When kidney function declines, erythropoietin production decreases, resulting in inadequate red blood cell formation despite normal bone marrow capacity.
Chronic diseases including liver disease, cancer, and persistent infections can suppress bone marrow function through inflammatory processes. These conditions interfere with normal bone marrow response, preventing appropriate increases in red blood cell production even when anemia develops.
Bone marrow suppression can also result from certain medications, particularly chemotherapy drugs, some antibiotics, and estrogen-containing compounds. Nutritional deficiencies affecting red blood cell production, while less common in dogs fed commercial diets, may contribute to non-regenerative anemia in cases of severe malnutrition or specific vitamin deficiencies. In cases of unexplained, non-regenerative anemia, bone marrow evaluation may be necessary to determine the underlying cause, especially when other diagnostic tests are inconclusive.
Common Causes of Anemia in Dogs
Parasites rank among the most frequent causes of dogs anemia, particularly in younger animals and those without consistent preventive care. Blood parasites including hookworms can cause significant blood loss, especially in puppies where even moderate infestations prove dangerous. Flea infestations, while seemingly minor, can drain substantial blood volume when populations become established, particularly affecting smaller dogs and those with compromised immune systems.
Tick-borne infections present serious risks for hemolytic anemia development. Ehrlichia and Babesia organisms transmitted through tick bites directly attack red blood cells, causing both destruction and suppression of bone marrow function. Lyme disease, also transmitted by ticks, can lead to anemia in dogs by causing joint swelling, arthritis, pain, and lameness. Geographic regions with higher tick populations see correspondingly increased rates of these infectious causes.
Toxic substances pose significant threats to red blood cell integrity. Human medications, particularly acetaminophen and ibuprofen, can cause severe hemolytic anemia in dogs even at relatively small doses. Common household items including onions, garlic, zinc-containing objects, and certain plants contain compounds that directly damage red blood cells or interfere with their function.
Chronic diseases affecting multiple organ systems frequently contribute to anemia development. Cancer, particularly blood cancers like leukemia and lymphoma, can directly infiltrate bone marrow or suppress normal blood cell production through systemic effects. Liver disease disrupts normal metabolism and protein synthesis essential for red blood cell health, while kidney disease reduces erythropoietin production necessary for stimulating new red blood cell formation.
Certain genetic disorders predispose specific breeds to anemia development. Basenjis may inherit pyruvate kinase deficiency, an enzyme disorder affecting red blood cell metabolism. West Highland White Terriers can develop hereditary disease affecting copper metabolism, leading to anemia through various mechanisms. These inherited conditions require specific genetic testing for accurate diagnosis and appropriate breeding decisions.
Diagnosis and Testing
Accurate diagnosis of anemia begins with a complete blood count, which measures red blood cell levels, hemoglobin concentration, and other essential blood parameters. This fundamental blood test provides the initial confirmation of anemia and helps classify its severity and type.
The packed cell volume test offers a quick assessment tool that veterinarians can perform in-clinic. Normal values typically exceed 35%, with measurements below this threshold indicating anemia of varying degrees. Severe anemia with PCV values below 20% often requires immediate intervention, while moderate anemia between 20-35% demands prompt investigation and treatment.
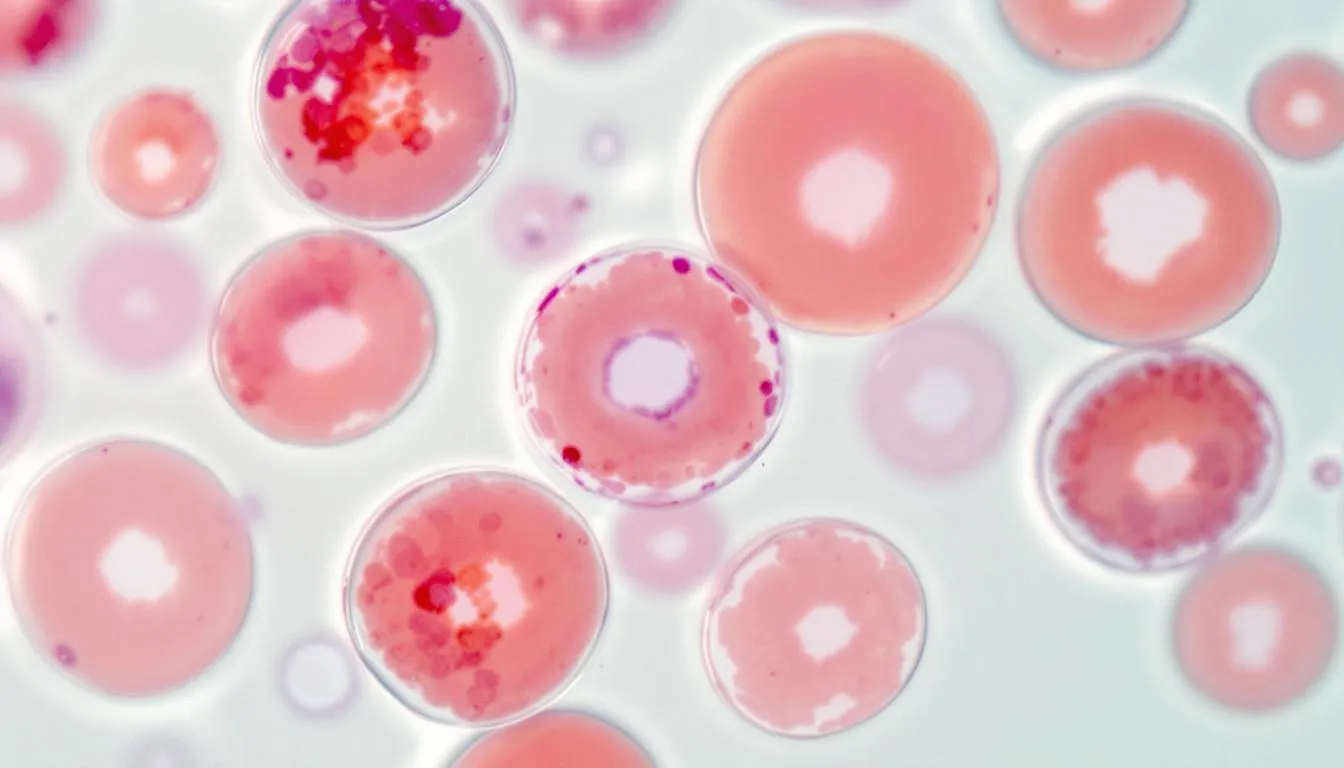
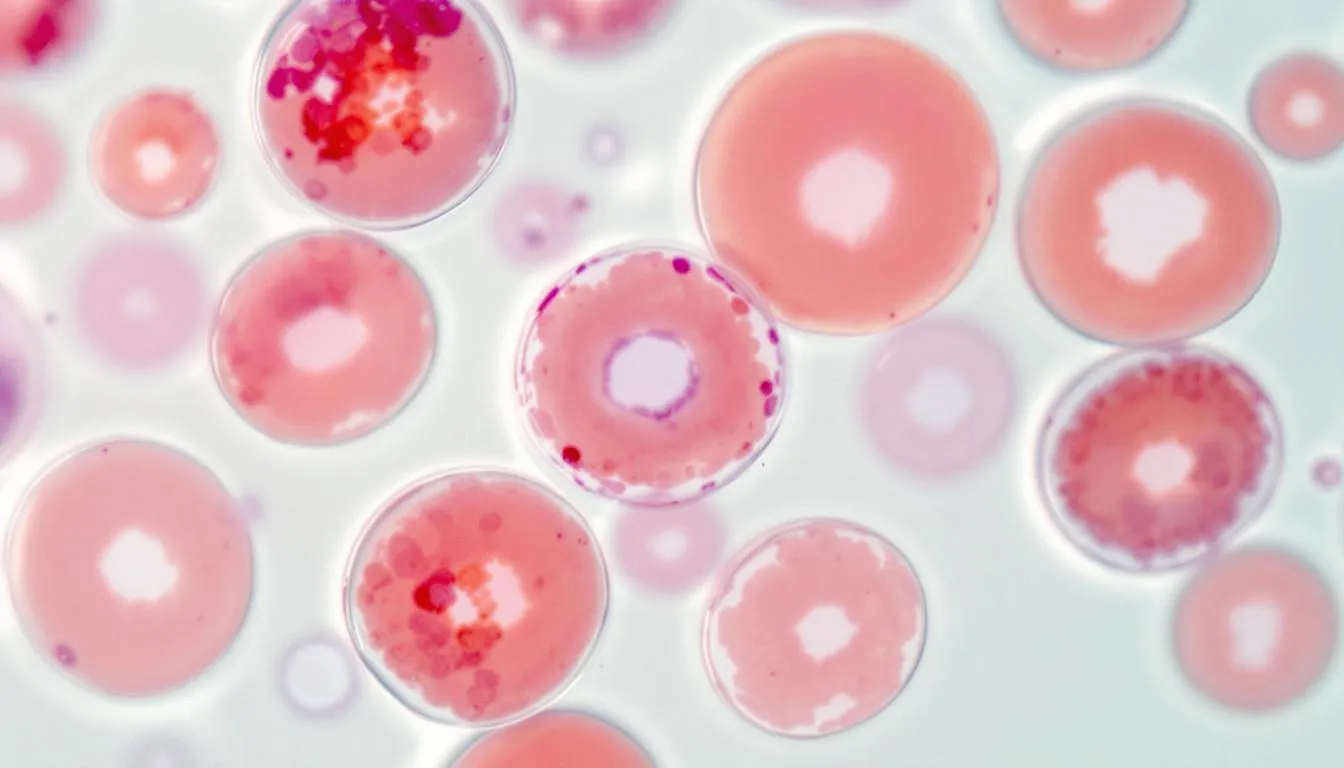
Blood smears provide detailed microscopic examination of red blood cell morphology, revealing important clues about underlying causes. These prepared slides allow veterinarians to identify blood parasites, assess cell shape and size variations, and detect abnormal cells that might indicate bone marrow disease or specific genetic disorders.
Automated blood analyzers offer comprehensive analysis including reticulocyte counts, which measure immature red blood cells recently released from bone marrow. Elevated reticulocyte counts suggest regenerative anemia where bone marrow responds appropriately to the anemic state, while low counts indicate non-regenerative anemia requiring different diagnostic approaches.
When initial blood tests suggest bone marrow disease or unexplained non-regenerative anemia, bone marrow biopsy may become necessary. This procedure involves collecting samples of bone marrow tissue for microscopic examination, allowing direct assessment of blood cell production capacity and identification of infiltrative diseases like cancer.
Additional diagnostic testing depends on suspected underlying causes. Imaging studies including radiographs and ultrasound help identify sources of internal bleeding or organ abnormalities. Specific tests for infectious agents, including PCR testing for tick-borne diseases, provide targeted diagnosis when parasitic or bacterial causes are suspected.
Anemia Diagnosed: What’s Next?
When your dog is diagnosed with anemia, the next step is to determine the underlying cause and create a personalized treatment plan. Your veterinarian may recommend blood transfusions to quickly restore red blood cell levels, especially in cases of severe anemia. Medications might be prescribed to address autoimmune conditions or infections that are damaging red blood cells. For dogs with non regenerative anemia, where the bone marrow isn’t producing enough new red blood cells, treatment may focus on stimulating bone marrow activity or managing related issues like kidney disease or bone marrow disease. Ongoing monitoring is crucial—regular complete blood counts and blood smears help track your dog’s progress and ensure that red blood cell production is improving. By identifying the underlying cause and closely monitoring your dog’s response, your veterinary team can adjust the treatment plan as needed to support recovery and long-term health.


Treatment Options for Canine Anemia
Treatment strategies for anemia must address both immediate stabilization needs and underlying disease processes. Blood transfusions become necessary for severe, life-threatening anemia where red blood cell levels drop dangerously low. These procedures require careful cross-matching to prevent transfusion reactions and should only be performed in equipped veterinary facilities with appropriate monitoring capabilities.
For autoimmune hemolytic anemia, immune suppression therapy represents the primary treatment approach. Corticosteroids like prednisone help reduce the immune system’s attack on red blood cells, though these medications carry risks including increased infection susceptibility and potential side effects requiring careful monitoring.
Iron supplementation proves essential for treating iron deficiency anemia, particularly cases resulting from chronic blood loss. However, iron therapy should only follow proper diagnosis, as excess iron can be harmful and ineffective treatment may delay identification of ongoing bleeding sources.
Dogs with kidney disease-related anemia may benefit from erythropoietin therapy, though this treatment requires careful monitoring for antibody development and potential complications. This hormone replacement helps stimulate red blood cell production when natural erythropoietin levels become insufficient.
Treatment of underlying infections, parasites, or chronic diseases forms the foundation of successful anemia management. De worming medications eliminate parasitic causes, while antibiotics address bacterial infections contributing to red blood cell destruction or bone marrow suppression.
Supportive care including fluid therapy helps maintain blood pressure and tissue perfusion while underlying treatments take effect. Oxygen supplementation may prove necessary in severe cases where oxygen delivery becomes critically compromised.
Managing Anemia in Dogs
Successfully managing anemia in dogs involves a combination of medical care, lifestyle adjustments, and preventive strategies. Dogs with chronic or severe anemia may require periodic blood transfusions to maintain healthy red blood cell levels, especially if their bone marrow cannot keep up with demand. For those with iron deficiency anemia, iron supplements and a healthy diet rich in essential nutrients are important to support red blood cell production. Preventing exposure to toxins and certain medications that can suppress bone marrow function is also critical. Regular de-worming helps protect against blood parasites that can contribute to anemia, while ongoing veterinary check-ups allow for early detection of complications or relapses. In cases involving liver disease, bleeding disorders, or other serious underlying conditions, hospitalization and intensive care may be necessary to stabilize your dog and provide further treatment. By working closely with your veterinarian and making thoughtful lifestyle choices, you can help manage your dog’s anemia and improve their quality of life.
Prevention Strategies
Year-round parasite prevention using veterinarian-approved products provides the most effective protection against many common causes of anemia. Modern flea and tick preventives offer broad-spectrum protection against blood-sucking parasites and disease-transmitting arthropods that can trigger both blood loss and hemolytic anemia.
Safe storage of human medications and toxic substances prevents accidental ingestion that can cause severe hemolytic anemia. Many cases result from dogs accessing dropped pills or improperly stored medications, making household safety measures essential for prevention.
Maintaining a healthy diet with high-quality commercial dog food ensures adequate nutrition for optimal red blood cell production. While nutritional anemia remains uncommon in dogs fed balanced commercial diets, proper nutrition supports overall bone marrow function and helps maintain healthy immune system responses.
Regular wellness examinations every 6-12 months allow early detection of conditions that might progress to anemia. These visits enable veterinarians to identify subtle changes in energy, appetite, or physical examination findings before severe anemia develops.
Certain breeds require extra monitoring due to genetic predispositions. Shih Tzus, Labrador Retrievers, and other breeds with higher autoimmune disease risks benefit from increased vigilance for early anemia symptoms. Responsible breeding practices including genetic testing help reduce hereditary disease transmission.
Avoiding known toxic foods like onions, garlic, grapes, and raisins prevents exposure to compounds that can trigger red blood cell destruction. Even small amounts of these substances can cause problems in sensitive dogs, making complete avoidance the safest approach.
Anemia Contact and Support
If your dog is living with anemia, staying in close contact with your primary care veterinarian is essential for effective management. Schedule regular follow-up appointments to monitor your dog’s condition, review blood test results, and adjust treatments as needed. Don’t hesitate to reach out to your veterinary team if you notice any changes in your dog’s health or if symptoms of severe blood loss or sudden blood loss occur—quick action can be life-saving. Connecting with support groups, both online and in your community, can provide valuable emotional support and practical tips from other pet owners facing similar challenges. Keep a list of emergency veterinary contacts handy in case your dog’s condition worsens unexpectedly. By staying informed, proactive, and connected, you’ll be better equipped to support your dog through the ups and downs of anemia and ensure they receive the best possible care.
When to Contact Your Veterinarian
Immediate emergency signs requiring urgent care include severe weakness or collapse, extremely pale or white gums, rapid or labored breathing, and any signs of bleeding that cannot be controlled. These symptoms suggest severe anemia requiring immediate medical intervention to prevent life-threatening complications.
Progressive symptoms that worsen over time warrant prompt veterinary evaluation even when initially mild. Gradual decreases in energy, appetite changes, or subtle gum color changes may indicate developing anemia that will respond better to early treatment than delayed intervention.
Dogs with diagnosed chronic diseases including kidney disease, liver disease, or cancer require routine monitoring to detect anemia development before it becomes severe. These underlying illness conditions predispose dogs to anemia, making regular blood work essential for optimal management.
Follow-up care after anemia diagnosis depends on the underlying cause and treatment approach. Dogs receiving immune suppression therapy need frequent monitoring for treatment response and potential side effects, while those recovering from blood loss require assessment of healing progress and red blood cell regeneration.
Contact your primary care veterinarian whenever you observe changes in your dog’s energy level, appetite, or general demeanor that persist beyond 24-48 hours. Early consultation allows for timely diagnosis and treatment initiation, which significantly improves outcomes for most types of anemia.
FAQ
How long does it take for a dog to recover from anemia?
Recovery time varies significantly depending on the underlying cause and severity. Dogs with blood loss anemia may show improvement within days to weeks once bleeding stops and iron therapy begins. However, autoimmune hemolytic anemia often requires months of treatment, and some dogs need long-term medication management. Anemia from chronic diseases like kidney failure typically requires ongoing management rather than complete cure.
Can puppies develop anemia differently than adult dogs?
Yes, puppies are particularly vulnerable to developing anemia from sources that might not severely affect adult dogs. Heavy parasite loads, especially hookworms and fleas, can cause life-threatening blood loss in young animals. Puppies also have less blood volume overall, making any blood loss more significant. Additionally, certain inherited conditions may manifest anemia symptoms earlier in life, requiring genetic testing for proper diagnosis.
Are certain dog breeds more susceptible to specific types of anemia?
Several breeds show increased predisposition to particular types of anemia. Cocker Spaniels, Miniature Schnauzers, and English Springer Spaniels have higher rates of immune mediated hemolytic anemia (IMHA). Basenjis may inherit enzyme deficiencies affecting red blood cell function, while West Highland White Terriers can develop copper metabolism disorders leading to anemia. Large breed dogs may be more susceptible to certain cancers that cause anemia.
What is the cost of treating anemia in dogs?
Treatment costs vary widely based on the underlying cause and severity. Basic diagnostic blood work typically ranges from $100-300, while comprehensive workups including imaging and specialized tests can exceed $1,000. Blood transfusions cost $300-800 per procedure, and ongoing medications for autoimmune conditions may require $50-200 monthly. Emergency treatment for severe anemia can reach several thousand dollars, making pet insurance and preventive care valuable investments.
Can anemia in dogs be completely cured or only managed?
The possibility of cure versus management depends entirely on the underlying cause. Anemia from parasites, infections, or toxic exposures often resolves completely with appropriate treatment. However, anemia from chronic diseases like kidney failure or genetic disorders typically requires lifelong management. Autoimmune hemolytic anemia may achieve remission with treatment, but recurrence remains possible, requiring ongoing monitoring even after apparent recovery.
FAQ
How long does it take for a dog to recover from anemia?
Recovery time varies significantly depending on the underlying cause and severity. Dogs with blood loss anemia may show improvement within days to weeks once bleeding stops and iron therapy begins. However, autoimmune hemolytic anemia often requires months of treatment, and some dogs need long-term medication management. Anemia from chronic diseases like kidney failure typically requires ongoing management rather than complete cure.
Can puppies develop anemia differently than adult dogs?
Yes, puppies are particularly vulnerable to developing anemia from sources that might not severely affect adult dogs. Heavy parasite loads, especially hookworms and fleas, can cause life-threatening blood loss in young animals. Puppies also have less blood volume overall, making any blood loss more significant. Additionally, certain inherited conditions may manifest anemia symptoms earlier in life, requiring genetic testing for proper diagnosis.
Are certain dog breeds more susceptible to specific types of anemia?
Several breeds show increased predisposition to particular types of anemia. Cocker Spaniels, Miniature Schnauzers, and English Springer Spaniels have higher rates of immune mediated hemolytic anemia (IMHA). Basenjis may inherit enzyme deficiencies affecting red blood cell function, while West Highland White Terriers can develop copper metabolism disorders leading to anemia. Large breed dogs may be more susceptible to certain cancers that cause anemia.
What is the cost of treating anemia in dogs?
Treatment costs vary widely based on the underlying cause and severity. Basic diagnostic blood work typically ranges from $100-300, while comprehensive workups including imaging and specialized tests can exceed $1,000. Blood transfusions cost $300-800 per procedure, and ongoing medications for autoimmune conditions may require $50-200 monthly. Emergency treatment for severe anemia can reach several thousand dollars, making pet insurance and preventive care valuable investments.
Can anemia in dogs be completely cured or only managed?
The possibility of cure versus management depends entirely on the underlying cause. Anemia from parasites, infections, or toxic exposures often resolves completely with appropriate treatment. However, anemia from chronic diseases like kidney failure or genetic disorders typically requires lifelong management. Autoimmune hemolytic anemia may achieve remission with treatment, but recurrence remains possible, requiring ongoing monitoring even after apparent recovery.






